Sharon Eve Sonenblum, PhD; Stephen H. Sprigle, PhD, PT
Rehabilitation Engineering and Applied Research Laboratory, Georgia Institute of TechnologyIntroduction
Pressure ulcers (PUs) are a leading secondary complication of spinal cord injury (SCI), affecting more than 50% of people with SCI at some point in their lives (Raghavan, Raza, Ahmed, & Chamberlain, 2003). Research into PU prevention can be generally categorized into two areas: risk assessment and PU etiology.
PU risk assessment tools (e.g., Braden, Norton) identify people who, if treated with standard care, are likely to develop an ulcer. Therefore, risk assessment tools inform the clinician which patients should be watched more closely but are not designed to inform clinicians about individualized interventions (Bolton, 2007). One challenge is that research has yet to directly link clinical risk factors to the more theoretical understanding of etiology. So the tools identify someone as at-risk, but do not provide for any understanding of why certain risk factors lead to PU development. Furthermore, within the at-risk populations, there are still people more likely to develop PUs than others. Therefore, this study seeks to define the nature of the influence of risk factors. With this knowledge, we intend to inform individualized PU risk assessment and prevention.
A large number of intrinsic characteristics have been identified as contributing to pressure ulcer risk. For this study, we identified 7 known pressure ulcer risk factors that we believed might impact tissue compliance or blood flow response to loading. These included level of injury (Byrne & Salzberg, 1996; Salzberg et al., 1998; Vidal & Sarrias, 1991), body mass index (BMI) (Allman, Goode, Patrick, Burst, & Bartolucci, 1995), blood pressure, smoking status (Byrne & Salzberg, 1996; Krause & Broderick, 2004; Raghavan et al., 2003; Sprigle, Linden, & Riordan, 2002), , hematocrit (Salzberg et al., 1996), serum albumin (Byrne & Salzberg, 1996; Salzberg et al., 1996) and lymphocyte count (Allman et al., 1995).
The goal of this study was to identify clinically-measurable characteristics that can be used to predict buttocks tissue response to loading. Specifically, we sought to identify how tissue compliance and blood flow was impacted by clinically-measurable risk factors.
Methods
35 young men with chronic SCI were enrolled in this study with IRB approval. This homogenous population was selected in order to limit variability across age, diagnosis, and gender, thereby increasing the power available to study other risk factors.
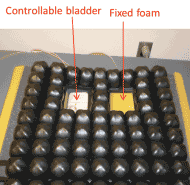 Figure 1 . Test cushion was used to control the pressure at the IT. (Reproduced from (Sprigle et al., 2013), modified to add text)
Figure 1 . Test cushion was used to control the pressure at the IT. (Reproduced from (Sprigle et al., 2013), modified to add text) To investigate the blood flow response to loading and unloading, a custom test environment was developed that allowed us to load and unload the ischial tuberosity (IT) region of participants’ buttocks while they sat in an upright posture. The custom wheelchair cushion contains a bladder under one IT region of a seated participant (Figure 1). Inflating and deflating the bladder provided full control over the pressure at the IT. Target interface pressures were identified using measurements from a small (3”x5”) Tekscan sensor adhered to the bladder. The superficial blood flow was measured by the PeriFlux 5010 Laser Doppler Perfusion Monitor (Perimed AB, Sweden) with a custom probe attached to the apex of the ischial tuberosity (Sonenblum & Sprigle, 2011).
The data collection protocol began with the IT unloaded for 5 minutes, followed by 2 minutes at a low load (40-60 mmHg) and 2 minutes at a high load (> 200 mmHg). This unloaded à low load à high load sequence was repeated 3 times. The Laser Doppler Flowmeter was configured to record the blood flow flux at a sampling rate of 32 Hz and the interface pressure sensor measured the interface pressure at 1 Hz.
After collection of blood flow data, subjects were lifted in the Guldmann net and the Doppler sensor was removed. Next the tissue compliance data was collected using the Myotonometer (Leonard et al., 2003). The Myotonometer is a handheld device used to apply a known load with a plunger, and the device measures tissue displacement. The Myotonometer was pushed vertically on the buttocks towards the IT by a trained clinician. The tissue was loaded to 1.5 kg and unloaded for 8 continuous cycles. This test was repeated 2 more times, with a rest period of 1 minute between tests.
Participants also filled out a survey addressing risk factors mentioned previously (i.e., BMI, level of injury, and smoking status). A clinician collected blood pressure to estimate the mean arterial pressure. Finally, the hospital’s phlebotomist drew blood and the lab’s serology results were used to evaluate total lymphocyte count, hematocrit, and serum albumin levels.
Data analysis was performed separately for tissue compliance and blood flow.
Tissue Compliance
The Myotonometer outputs the tissue displacement at fixed loads, allowing for the calculation of a number of different metrics. Because we were interested in two different constructs of tissue properties – stiffness and thickness – we chose to study two orthogonal metrics that are related to these constructs.
- ButtocksDisplacement: the displacement of the buttocks tissue at the apex of the IT with the application of 0.43 kg of load; and
- %MaxDisplacement: the % of maximum displacement (i.e., displacement occurring at 1.5 kg) present at 0.43 kg. This is a measure of how “bottomed out” the tissue is at 0.43 kg.
Two stepwise regression models were run with 5 risk factors as inputs (level of injury, BMI, mean arterial pressure, smoking status, and lymphocyte count) and the median ButtocksDisplacement and %MaxDisplacement from the 3 trials as outputs. P<0.05 was selected for inclusion of a variable. The remaining two variables (hematocrit and serum albumin) were not included in the modeling because almost all subjects had normal levels, and the variability across subjects was very small.
Blood flow
Blood flow signals were filtered with a 2nd order, low pass Butterworth filter with a cutoff frequency of 1 Hz. Blood flow was further analyzed by taking the average flow from the final 60 seconds in the low and high loaded conditions and dividing by the preceding unloaded blood flow to produce a normalized blood flow. Normalized blood flow is important because Laser Doppler measures blood flow in arbitrary units, making comparisons of absolute measures across subjects more difficult than relative changes.
Two stepwise regression models were run with the 5 risk factors (level of injury, BMI, mean arterial pressure, smoking status, and lymphocyte count), ButtocksDisplacement, and %MaxDisplacement as inputs and the median normalized blood flow (low and high pressure conditions) from the 3 trials as outputs. P<0.05 was selected for inclusion of a variable.
Results
As per the inclusion criteria, all participants were male ages 20-40 and were more than 2 years post SCI (Table 1). Participants included 16 cervical level injuries and 19 non-cervical injuries. The average participant was considered to have a healthy weight, with a mean BMI of 24.2 (range 15.6-37.9). Ten participants were current smokers, although more than 20 had been smokers at some point in time. The average lymphocyte count was 1720 ± 540 cells/µL. With lymphopenia occurring when the lymphocyte count falls below 1500 cells/µL, 14 participants were defined as having lymphopenia. Finally, the average mean arterial pressure of 87.7 is considered normotensive, although it is approaching hypertensive (Miller, Rosales, Kelly, & Henry, 2005).
Characteristic |
Mean (SD) or n (%) |
Age |
31 (5) |
Years post injury |
10 (5) |
BMI |
24.2 (5.3) kg/m2 |
Cervical Injury |
16 (46%) |
Current Smokers |
10 (29%) |
Mean Arterial Pressure |
87.7 (15.5) mmHg |
Lymphocyte Count |
1720 (540) cells/µL |
Hemoglobin |
14.2 (1.1) g/dL |
Serum Albumin |
4.1 (0.3) g/dL |
Tissue Compliance
Across 35 subjects, the ButtocksDisplacement at 0.43kg was 9.5 ± 2.5 mm. At 0.43 kg of load, the %MaxDisplacement was 80.4 ± 7.5% of the maximum displacement. ButtocksDisplacement ranged from 3.4 mm – 15.2 mm, and %MaxDisplacement from 63.8 – 96.1%.
In the regression model for ButtocksDisplacement, only BMI was related to the amount of buttocks displacement (β = 0.267, 95% CI [0.123,0.411]). In other words, increasing BMI by 5 kg/m2, or crossing from normal to overweight, or overweight to obese, resulted in an additional 1.3 mm of displacement (or an increase in displacement by almost 15%). The model for %MaxDisplacement also included only one risk factor - smoking status (β = 0.071, 95% CI [0.019, 0.123]). Current smokers experienced 86 ± 5% of maximum displacement at 0.43kg, compared with only 79 ± 7% for non-smokers.
Blood Flow
Blood flow data was collected for 34 subjects, as one subject did not complete the study. Blood flow did not experience a significant change from unloaded when a low load was applied to the buttocks (Table 2). At high loads, however, blood flow was significantly reduced.
| Loading Condition | Mean (SD) | CoV |
|---|---|---|
Low |
1.07 (0.69) |
59.3% |
High |
C0.28 (0.38) |
104.5% |
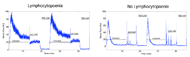 Figure 2. Example blood flow response for individuals with and without lymphopenia. Reproduced from (Sprigle, Sonenblum, & Conner-Kerr, 2013)
Figure 2. Example blood flow response for individuals with and without lymphopenia. Reproduced from (Sprigle, Sonenblum, & Conner-Kerr, 2013) Regression modeling to predict blood flow responses was made difficult by the high inter-subject variability (Table 2). Only one of the risk factors identified a priori had a significant role in the regression models at low load – lymphopenia. As reported briefly in Sprigle, et al. (Sprigle et al., 2013), subjects with lymphopenia experienced significantly higher blood flow during unloaded sitting, a slower decay from the peak hyperaemic response, and a lower normalized pressure at low load (Figure 2). In fact, while subjects without lymphopenia experienced no significant change from unloaded during low loads (blood flow = 1.20 ± 0.62, 95% CI [0.93, 1.47]), subjects with lymphopenia did experience a significant drop in blood flow during low loads (blood flow = 0.66 ± 0.38, 95% CI [0.40, 0.91]). None of the risk factors was found to be significant in the models for blood flow at high load.
Discussion
The buttocks’ response to loading is a critical factor in pressure ulcer development. This study selected a homogenous population – young men with chronic SCI – in order to study other risk factors, and found considerable variation in the buttocks response across individuals. Clinically, this implies that two young men with SCI who present fairly similarly on first inspection may be at very different risk of PU development. Therefore, they may have very different needs in terms of cushion prescription and pressure relief interventions.
The precise mechanisms by which internal loading and physiological responses lead to pressure ulcers are not known, however current evidence suggests that damage can result directly from the deformation (Bouten, Oomens et al. 2003, Gawlitta, Li et al. 2007), or the result of impairment to blood flow that results from deforming tissue under load (Sanada, Nagakawa et al. 1997, van Marum, Meijer et al. 2002). Therefore, tissue that is more prone to deformation during sitting is likely to be at greater risk for PU development. This study found that ButtocksDisplacement, a measure of tissue compliance, varies with BMI. More overweight individuals experienced greater deformation of the bulk tissue at the IT, explaining one reason why individuals with high BMIs are considered to be at risk for PU development. Unfortunately, this study did not include a large enough population of underweight individuals (n=3) to assess how tissue compliance changes with low BMI values.
Another interesting conclusion was that %MaxDisplacement, which is related to how quickly the tissue reaches maximum deformation, was impacted by smoking. Being a smoker resulted in the tissue bottoming out at a lower load than non-smokers, meaning there is less cushioning left in the tissue to react when greater loads are experienced. The loss of this safety factor could result from degradation of elastic fibres in the tissue (Just, Ribera, Monso, Lorenzo, & Ferrandiz, 2007), and suggests that the mechanism by which smoking impacts PU development extends beyond its impact on blood flow responses (Sprigle et al., 2002).
Superficial blood flow responses to loading experienced even greater variability across subjects, making statistical modeling very difficult. At high loads, blood flow was significantly impaired for most subjects. Because most individuals experience such an extreme reduction in blood flow at high loads, it may not be valuable to further interrogate differences in responses at high loads. Of greater importance is studying the varied response to loading at low loads.
At low loads, the blood flow response varied according to subjects lymphocyte count. Interpreting this specific result presents a challenge, as illustrated in Figure 2. The impact of lymphopenia (or possibly a covariate that has not been investigated) could be to reduce the blood flow at low loads, or to extend the duration of the hyperaemic response and delay the return to steady state. These differences in responses at low loads are important, as the benefits of in-chair movements (which partially reduce seated pressure) might vary according to risk factors, as might the amount of time needed for blood flow to reach steady state.
Future Directions
Although there are many clinically measurable risk factors that might relate to how the tissue responds to loading, a small subset needed to be selected for this study to ensure sufficient statistical power. Therefore, many potentially important variables were not investigated. The next step for this research is to pursue an exploratory analysis of the impact of other factors such as age, time since injury, pressure ulcer history, and skin color on the tissue response to loading.
Conclusions
The goal of this study was to identify clinically-measurable characteristics that can be used to predict buttocks tissue response to loading. From the small set of variables studied, BMI and smoking status were found to relate to tissue compliance, while lymphocyte count was related to the blood flow response to low loads.
Acknowledgements
We would like to acknowledge Michelle Nemeth for her assistance with subject recruitment and data collection, and Bill Delaune for his assistance with the statistical analysis.
This work was completed as part of the Mobilitiy RERC, which is funded by the National Institute on Disability and Rehabilitation Research of the U.S. Department of Education under grant number H133E080003.
Audio Version PDF Version