Patterns in Wheeled Mobility Skills Training, Equipment Evaluation, and Utilization: Findings from the SCIRehab Project
Julie Gassaway, MS, RN1; Sally Taylor, PT, DPT, NCS2; Audrey Natale, PT, DPT3
1Shepherd Center; 2Rehabilitation Institute of Chicago; 3Craig Hospital
abstract
This study describes the type and quantity of manual and power wheelchair (WC) skills training provided for patients with traumatic spinal cord injury (SCI). It explores the process of wheeled mobility evaluation/prescription, and reports utilization and satisfaction with WC at the one-year injury anniversary. Occupational therapists (OTs) and physical therapists (PTs) documented treatment sessions during inpatient rehabilitation; one-year post injury outcomes were gathered by interview. Most patients participated in WC skills training; variation in type and frequency of WC skills training exists. Propulsion/driving skills were practiced most frequently. A majority of patients participated in wheeled mobility equipment evaluations; assessment/prescription and fitting were more frequently performed than mat evaluations. Most patients continued to use their WC and were satisfied with its fit and function at the one-year injury anniversary.BACKGROUND
According to the National Spinal Cord Injury Statistical Center (NSCISC), approximately 12,000 new cases of traumatic spinal cord injury (SCI) occur in the United States (US) each year (NSCISC, 2012). As a result of the trauma, most people with SCI will require some form of wheeled mobility to assist with activities of daily living (NSCISC, 2012).
PURPOSE
The aims of this proposal are to describe 1) the type and quantity of WC skills training provided by OTs and PTs during inpatient SCI rehabilitation by neurological level of injury (NLI), 2) methods used to determine WC prescription, and 3) patient satisfaction with and continued utilization of the WC at the one-year injury anniversary.
METHODS
The SCIRehab project, funded by the National Institute on Disability and Rehabilitation Research, is a practice-based evidence (PBE) research collaboration among six US inpatient rehabilitation centers specializing in the care for patients after SCI. It provides a unique opportunity to examine WC skills training provided during inpatient rehabilitation and the wheeled mobility equipment provision process in detail (Whiteneck, 2013). PBE methodology utilizes an observational cohort design focusing on treatment process and relates naturally occurring variation in treatment to outcomes, after controlling for patient demographic and injury characteristics (referred to as patient characteristics) (Horn, 2010).
Results
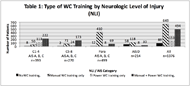
WC Skills training.
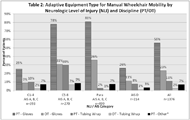
Wheeled Mobility Evaluation.
WC Satisfaction.
Most patients (81%) who reported receipt of a manual WC also reported continued use of the WC at one-year post injury and 87% of these patients were satisfied with the chair’s fit and function. Similarly, 86% of patients who were still using their power WC at one-year post injury were satisfied with its fit and function.
DISCUSSION
OTs and PTs focused a significant number of sessions on WC mobility training and most patients received wheeled mobility evaluations during inpatient SCI rehabilitation. Patients with tetraplegia (American Spinal Injury Association Impairment Scale (AIS) A,B,C) typically received about the same amount of training in both manual and power WCs, whereas manual WC training far exceeded power WC training among patients with paraplegia. Fewer patients with AIS D injuries received WC training and those who did were more likely to use manual than power equipment.
According to Rehabilitation Engineering and Assistive Technology Society of North America (RESNA Position Papers, 2011) guidelines, trialing multiple types of both manual and power WCs is required to determine best fit for overall function and patient needs. However, some patients begin mobility training in a power WC while regaining the necessary shoulder strength to meet the demands of manual WC propulsion or independent performance of pressure reliefs. Once upright sitting tolerance, strength, and management of pressure reliefs has improved, manual mobility training can be initiated. Therefore, overall time spent in WC mobility training is typically greater for these patients to address both power and manual skills. For others, manual mobility training is not pursued until they are in an outpatient setting.
The majority of WC mobility training time was spent on instruction of propulsion/driving of both manual and power WCs. Propulsion included navigation of a variety of surfaces including smooth and rough terrain and inclines, which are the most frequent terrains encountered in home and community settings. Patients with high tetraplegia likely require use of alternative powered drive control systems that may have a higher learning curve to master than more intuitive hand drives. Some patients, for example those with C5 LOI, may transition from alternative drive control systems to hand drive as shoulder musculature strengthens; skilled instruction must be provided to promote correct mechanics to avoid injurious compensatory strategies. For patients with low tetraplegia and paraplegia (C5 and below), therapists emphasize the practice of correct manual WC propulsion technique to decrease the incidence of upper extremity overuse injuries from highly repetitive motions.
The completion of most wheeled mobility equipment evaluations included WC assessment/ prescription and fitting; formal mat evaluations were used much less often. A mat evaluation can be both time and labor intensive when working with patients who may be physically dependent for transfers and mobility and the amount of time and personnel allotted for formal equipment evaluations may be a determinant of whether the evaluation occurs. Lack of mat evaluations does not devalue their importance but suggests that clinicians may be getting necessary information for definitive WC prescriptions from other less time-intensive or costly means. The patient’s posture, sitting balance, strength, range of motion and tone, for example, can be assessed as part of other therapeutic treatment activities. Body dimensions and anatomical alignment may be obtained while making adjustments to and trialing various WCs during the inpatient rehabilitation stay. Therefore, the lack of recorded mat evaluations does not indicate inadequate WC evaluations for patients.
While most patients reported continued use of prescribed WCs at the one-year injury anniversary and expressed satisfaction with the WC, approximately 13-14% expressed some dissatisfaction with the use of their WC. The phone interview question “Are you satisfied with the fit and function of your wheelchair?” included only a yes/no response and did not allow for discernment of specific areas of concern. The patient’s dissatisfaction could arise from factors such as inadequate equipment set up or adjustment, lack of follow up training with the WC, poor WC fit due to changes in patient condition/size, inferior equipment maintenance/condition, or inappropriate equipment selection.
Future Studies.
Future studies on WC procurement could focus on relationships of patient satisfaction with the fit and function of wheeled mobility devices with the type of mobility training and equipment evaluation performed during inpatient rehabilitation. Approximately 13% of patients expressed dissatisfaction with the fit and function of their WC by one year post injury; this suggests the need for further examination of appropriate equipment training, evaluation, and prescription at the time of discharge and reevaluation of WC fit as time progresses to ensure optimal fit of the equipment to promote use.
Limitations.
The six SCIRehab centers are not a probability sample of rehabilitation facilities across the United States that provide care for patients with SCI; therefore, findings may not be generalizable to all rehabilitation centers.
Treatment data collected were supplemental to required clinical documentation at each facility. While a variety of efforts were made to maximize completeness, including cross-checking with billing records and clinical documentation of therapy delivered as well as communications with clinical staff, it is expected that some treatment activities that occurred are not represented. Self-reported one-year post injury data may be subject to response and/or recall bias, resulting in underreporting or over reporting on some items.
After SCIRehab study data collection was completed in 2009, new best practice guidelines regarding wheeled mobility equipment evaluation and WC skills training (RESNA Position Papers, 2011) were released. Thus, data presented here may not reflect recent changes in treatment approaches.
conclusions
During inpatient rehabilitation, WC mobility training included many skills required for transition to independent mobility in the community; however, the greatest emphasis was on propulsion for both manual and power WC training. In order for the therapists to determine appropriate and safe mobility equipment after discharge from inpatient rehabilitation, the majority of patients participated in equipment evaluations. The most frequent activity performed was WC fitting, while mat evaluations were used infrequently. At one year post injury, most patients were satisfied with the fit and function of their manual and power WCs, and were still using their WC. Variation in the type and frequency of WC training provided by level of SCI and type of WC ordered for community use provides a foundation for future research to determine the best type of wheeled mobility training and equipment evaluation and to relate treatment modalities with functional and participation outcomes.
References
Horn, S. D., & Gassaway, J. (2010). Practice based evidence: incorporating clinical heterogeneity and patient-reported outcomes for comparative effectiveness research. Med Care, 48(6 Suppl), S17-22. doi: 10.1097/MLR.0b013e3181d57473
National Spinal Cord Injury Statistical Center. (2012). Data collection syllabus for the national spinal cord injury database:2008-2011 project period. Birmingham 2011. Spinal cord injury facts and figures at a glance. Retrieved July 3, 2012, from http://www.nscisc.uab.edu/PublicDocuments/fact_figures_docs/Facts%202012%20Feb%20Final.pdf.
Rehabilitation Engineering and Assistive Technology Society of North America. (2011). RESNA WC Service Provision Guide. Retrieved December 21, 2014, from http://www.resna.org/sites/default/files/legacy/resources/position-papers/RESNAWheelchairServiceProvisionGuide.pdf
Whiteneck, G, & Gassaway, J. (2013). SCIRehab uses practice-based evidence methodology to associate patient and treatment characteristics with outcomes. Arch Phys Med Rehabil, 94(4 Suppl), S67-74. doi: 10.1016/j.apmr.2012.12.022