Lung Capacity and Airflow Change Due to Different Sitting Posture.
ABSTRACT
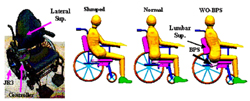
Individuals with spinal cord injury (SCI) exhibit reduced lung volumes and flow rates as a result of respiratory and abdominal muscle weakness. The compromised lung capacity may be worsened further when individuals with SCI remain seated for a long time in a Slumped posture, resulting from posterior pelvic and poor trunk support in the wheelchair . Changes in forced vital capacity (FVC), forced expiratory volume in 1 s (FEV 1 ), Forced Expiratory Ratio(FER) and Peak Expiratory Flow (PEF) were assessed in healthy subjects in three different seated postures; the Normal , Slumped , and the WO-BPS (without ischial support and with lumbar support ) posture provided by our new seating design. Results showed that the Slumped posture significantly reduced the lung capacity, compared with that of Normal and WO-BPS postures. The WO-BPS posture was slightly more effective than Normal posture in improving lung capacity of seated individuals, and increasing lumbar lordosis.
KEY WORDS:
Lung capacity, sitting, spirometer, Spinal cord injury
INTRODUCTION
Individuals with SCI can experience a range of complications that result from prolonged sitting with poor postural support. Reduced lung capacity (1) , back pain, and pressure ulcers are among the most common complaints. Additionally, pneumonia, influenza, and other respiratory illnesses are the leading cause of death of individuals with SCI (2) . Studies relating body posture and lung volume have been performed, but they focus almost exclusively on comparisons between sitting, prone, and supine postures, and significant changes were attributed to the weight of organs on the diaphragm (1) , or of shifts in what parts of the body blood pools in (3). No investigation was found to address the relationship between lung capacity in different postures in a seated individual. Based on the hypothesis that the lung capacity may be decreased when the individual remains seated in poor, Slumped posture, research was carried out to evaluate the relationship between the lung capacity measures and the sitting postures, which were chosen as Slumped , unsupported Normal and the WO-BPS . The evaluated lung capacity measures were the forced vital capacity (FVC), forced expiratory ratio (FER), peak expiratory flow (PEF), and forced expired volume in one second (FEV1). Lateral radiographic images were also used to measure the true spinal orientation, and to measure total lumbar lordosis.
METHODS:
 |
|---|
Protocol:
Each subject was directed to sit in the wheelchair in each posture. She/he was then asked to take the deepest breath possible and exhale hard into the transducer tube of the spirometer. This was repeated in other postures and three times in each posture. A brief rest of 30s between trials was used to minimize the fatigue effect on the lung capacity. The posture testing sequence was randomized according to a randomization schedule generated beforehand. A set of lateral sagittal plane radiograph of the lower spine, thigh, and pelvis was taken for both Standing and sitting postures ( Slumped , Normal and WO-BPS). The radiographic images were used to locate several bony landmarks and calculate total lumbar lordosis (4) .
After each subject completed the breathing measurements, these values were averaged to produce the mean and standard deviation of the FEV1, FVC, FER, and PEF for each subject in each posture. The total lumbar lordosis was measured for each subject using the Cobb method. The average and standard error of these values for all subjects were then calculated to produce the mean values for each posture. A t -test was used to calculate the significance level of these differences
Statistical Analysis:
Comparisons for the average values of FEV1, FVC, FER, and PEF were made between the Normal , WO-BPS , and Slumped postures. Analysis of variance was performed and pair-wised comparison was used to test whether there were significant differences between the postures. The significance level was set at 0.05. SAS software (SAS Institute, Cary , NC ) was used to perform the statistical analysis
RESULTS
The overall average values of the FEV1, FVC, FER, and PEF across all subjects for the Slumped , Normal , and WO-BPS postures are given in Table 1. The Normal and WO-BPS postures were produced almost identical readings.
Sitting Posture |
FEV1 |
FVC |
FER |
PEF |
|---|---|---|---|---|
Normal * P |
3.2± 0.2 0.171 |
3.8± 0.2 0.191 |
83.4± 2.2 0.399 |
415.8± 25.7 0.457 |
WO-BPS ** P |
3.3± 0.2 <0.001 |
3.9± 0.2 <0.001 |
83.6± 1.9 0.386 |
414.3± 30.4 <0.001 |
Slumped *** P |
2.9± 0.2 <0.001 |
3.47± 0.2 <0.001 |
83.89± 2.3 0.310 |
369.83± 29.4 <0.001 |
* P is the significance between values between the Normal and WO-BPS postures. ** P is the significance between values between the WO-BPS and Slumped postures. *** P is the significance between values between the Normal and Slumped postures. |
||||
Relative to the Normal and WO-BPS postures, the Slumped posture produced significantly ( P <.001) reduced FEV1, FVC and PEF with 2.94 ± 0.81L, 3.47 ± 0.18L, and 369.83 ± 29.38L/min, respectively. The FER readings were consistent throughout the tests, regardless of posture (Table 1).
The total lumbar lordosis of the spine changed greatly between virtually all postures, as seen in Table 2. Lordosis increased progressively, from the Slumped , to Normal , to WO-BPS , to Standing .
Postures |
Total Lordosis |
|---|---|
Slumped *P |
21.8±4.5 P =0.493, 0.024, 0.003 |
Normal **P |
22.4±4.0 P =0.003, P <0.001 |
WOPBS ***P |
42.5±1.5 P =0.001 |
Standing |
60.3±2.1 |
* P is the significance between values between the Slumped and the Normal , WO-BPS and Standing postures, respectively. ** P is the significance between values between the Normal , and the WO-BPS and Standing postures, respectively. *** P is the significance between values
between the WO-BPS and Standing postures |
|
DISCUSSION
These findings show that there is a significant decrease in airflow when a subject is slumping. This would compound any preexisting breathing difficulties an individual with SCI would experience because of reduced muscle strength and control, as their breathing abilities would be further compromised. It is therefore important for people with SCI with respiratory issues to maintain proper posture to the fullest extent possible to prevent additional reductions in lung capacity. Furthermore, the WO-BPS posture was as effective at promoting high FEV1 and FVC values as the Normal sitting posture, indicating that this posture does not compromise a person's airflow.
Additionally, we found that WO-BPS posture increased total lumbar lordosis. This is not the case the Slumped posture, which did not increase lordosis, as seen in Table. 2. This position may compress organs and impede diaphragm movement. Decreased lordosis may account for the changes in capacity in the different postures, and the normal lung capacity in the WO-BPS posture, as the adjusted postures may change the volume available to the lungs, or allow the diaphragm and other respiratory muscles to function with different efforts.
The changes in FEV1, PEF, and FVC between the Normal and WO-BPS show no significant differences. This may be due to the short measurement period. Longer recording times may facilitate comparisons between the two postures.
The FER of all tests remained largely unchanged. As FER is an indicator of what percentage of the lung volume is being exhaled per second it is expected to change very little, as it will typically only change in the event of airway blockage, or as a result of smoking (3) . This steady ratio is consistent with many previous studies into respiratory behavior (1, 5) .
Improvements in seating could have dramatic effects on the quality of life of individuals in a wheelchair by improving posture, facilitating motion, decreasing pain, and preventing musculoskeletal disorders in people with SCI.
CONCLUSIONS
The results indicate that the Slumped posture will impair breathing, and should be prevented to ensure proper breathing, while the WO-BPS position promotes good posture, and does not reduce lung capacity. Further studies are necessary to determine the actual therapeutic value of the WO-BPS seating posture. These studies should include recordings of these trials over longer periods, and the inclusion of more subjects, including those with SCI to gauge actual benefits. It is also worth including several functional tasks, such as reaching, to test the effect of the seating configurations on mobility.
REFERENCES
- Chen, C.F., I.N. Lien, and M.C. Wu, Respiratory Function in Patients with Spinal Cord Injuries: Effects of Posture. Paraplegia, 1990. 28 : p. 81-86.
- Frankel, H.L., et al., Long Term Survival in Spinal Cord Injury: A Fifty Year Investigation. Spinal Cord, 1998. 36 : p. 26674.
- Baydur, A., R.H. Adkins, and J. Milic-Emily, Lung Mechanics in Individuals with Spinal Cord Injury: Effects of Injury Level and Posture. J. Appl. Physiol., 2001. 90 : p. 405-11.
- Makhsous, M., et al. SITTING PRESSURE IN A WHEELCHAIR WITH ADJUSTABLE ISCHIAL AND BACK SUPPORTS . in RESNA 26th International Conference . 2003. Atlanta, GA.
- Morgan, M.D.L. and J.R. Silver, The Respiratory System of the Spinal Cord Injuries . Management of Spinal Cord Injuries, ed. R.F. Bloch and M. BasaBaum. 1986, Baltimore: Williams & Wilkins.
ACKNOWLEDGEMENTS
The project was supported in part by PVA (Paralyzed Veterans of America) Award #2321-01, and Falk Medical Research Trust. Special thanks go to Jessica Penderson.
Author Contact Information:
Mohsen Makhsous, PhD,
Rehabilitation
Institute of Chicago,
345 E. Superior St., Chicago, IL 60611,
Office Phone 312-238-4824,
EMAIL: m-makhsous2@northwestern.edu
