29th Annual RESNA Conference Proceedings
Feasibility of Dynamic Pedobarography to Evaluate Ankle Foot Orthotics Following Brain Injury
Karen J. Nolan, PhD1,2 , Lisa K. Simone, PhD1,2 , Howard J. Hillstrom, PhD3 , Sue A. Sisto, PhD1,2 , Elie P. Elovic, MD1,2
1. Kessler Medical Rehabilitation Research and Education Corporation, West Orange, NJ USA
2. University of Medicine and Dentistry, New Jersey-NJ Medical School, Newark, NJ USA
3. Hospital for Special Surgery, New York, NY USA
ABSTRACT
Ankle Foot Orthotics (AFOs) are traditionally prescribed to improve an individual's gait following acquired brain injury. While AFOs help compensate for common problems such as foot drop (inadequate ankle dorsiflexion) or inappropriate foot strike due to spasticity or contracture, AFOs can cause pain, discomfort, and skin breakdown if not fitted properly. Currently, fit and improvements in gait are evaluated visually and corrected after patient feedback. However, a method to evaluate fit and gait changes objectively at the time the AFO is prescribed could improve outcomes and reduce malalignment issues. A wearable pedobarography system was used to evaluate the differences in dynamic pressures across the plantar surface of the foot when subjects walk with and without their previously prescribed AFOs. Initial results show significant differences in foot pressure were found during the push off phase, indicating that the observed improvements in gait due to the AFO can be measured objectively.
KEYWORDS:
foot pressure, orthotic, hemiplegia, stroke, pedobarography, outcome measures
BACKGROUND/PURPOSE
Brain injury due to stroke occurs every 45 seconds in the United States. This accounts for over 700,000 strokes each year, leaving 4.7 million stroke survivors alive today (1). Stroke is the leading cause of serious long term disability in the United States; significant functional limitations in activities of daily living, such as walking, occur as a result of stroke (1). Half of survivors had some hemiplegia, a paralysis that primarily affects only one side of the body following stroke, and 30% were unable to walk without some assistance (2,3).
Walking or gait patterns in hemiplegia have characteristic alterations. These disturbances in normal walking patterns can cause slower walking speed, shorter step length, foot drag, and perturbations in balance (3-5). The braking (foot strike) and propulsive (push off) phases of the gait cycle are inefficient in hemiplegic gait. This is often due to inefficient weight bearing and shorter stance duration on the affected side (6). During the swing phase hemiplegic patients often have difficulty clearing the floor due to inadequate ankle dorsiflexion, commonly referred to as "drop foot" (3,4). Hemiplegic patients also have less dorsiflexion during heel strike and mid-swing due to loss of motor control, spasticity of the gastrocnemius-soleus group, and ankle contracture. As a result the affected side often strikes the ground with the toes or sole of the foot rather than the heel (3,6).
Hemiplegic gait is commonly treated using an assistive device such as wheelchair, walker, cane, brace, or orthotic. Ankle foot orthotics (AFOs) are prescribed to hemiplegic stroke patients to provide optimal ambulation (3). The AFO is designed to help compensate for the mediolateral instability of the ankle joint, allow for a better heel strike, and prevent foot drop by restricting plantarflexion to provide a more effective push off (3,4,7,8). When properly prescribed, AFOs can be very beneficial to the gait of a hemiplegic patient; over 4 million Americans use some type of AFO. There are, however, some potential problems with prescription and use of AFOs.
Most AFOs are still prescribed solely based on visual observation to interpret human locomotion. Observing gait typically reveals compensations or symptoms of underlying pathologies, but is limited to the experience of the clinician. In addition, visual inspection may not identify aberrant loading patterns that can lead to pain, discomfort and ultimately skin breakdown on the plantar surface of the foot. Many research studies have revealed individual characteristics of hemiplegic gait but have not included information regarding the changes in foot pressure and load inside the shoe between the foot and the AFO (9). It is important to understand what affect the AFO has on forces, and pressures acting between the foot and support interface to get a complete picture of how the AFO affects the patient.
One method proposed to address these problems is the use of dynamic pedobarography, or the objective measurement of pressures on the plantar surface of the foot. One technology includes a wearable device and instrumented foot insoles with nearly 100 pressure sensors each. This innovative foot pressure technology can provide a wealth of information regarding foot pressure versus location on the foot, and also pressure changes during specific phases of the gait cycle such as push off and foot strike. While observational gait analysis can be used to determine if the AFO makes a patient's gait look better, instrumented pedobarography can add objectivity by allowing clinicians to assess the positive or negative affects of these changes. High pressure areas and poor gait characteristics due to malalignments can be detected and corrected before a pressure sore or other orthopedic foot injury develops.
The use of pressure sensors between the foot and support surface interface also provides objective information regarding how the individual structures of the foot are loaded as they come in contact with the supporting surface (10). This information enhances the clinician's ability to evaluate how load bearing of different foot structures is modified (9), in order to improve foot function by helping to train and control load during foot strike and push off, as well as help to realign and stabilize the foot and ankle after stroke (9).
The purpose of this research is to determine if dynamic pedobarography is a feasible method of evaluating the affect of an AFO on the plantar surface of the foot by measuring maximum pressure different phases of the gait cycle. For this pilot analysis, we have focused on peak pressures during the push off phase in hemiplegic stroke patients.
METHODS
Five individuals with hemiplegia resulting from stroke were recruited for participation. All were at least 6 months post stroke and used a prescribed custom molded plastic AFO during ambulation. Subjects performed walking trials in two different conditions: 1) (+)AFO: while wearing the AFO, and 2) (-)AFO: without the AFO. During data collection, all subjects were recorded while completing 10 walking trials, each consisting of a 4.5 meter walk at a self-selected walking speed. Five walking trials were collected in both the (+)AFO and (-)AFO condition for a total of 10 trials. The order of conditions was randomly assigned. Sock type was standardized for all subjects to minimize shear friction and plantar pressure attenuation caused by low pass filtering effects of the material. All activities were performed at a self selected pace; subjects were permitted to take breaks at any time during testing to minimize fatigue.
During all walking trials, foot pressure data was collected using pedobarography via the Pedar ® -x Expert System (Novel Electronics Inc., St Paul, MN, USA). The Pedar ® -x is an accurate and reliable pressure distribution measuring system for monitoring local loads under the foot (11,12). The system consists of a portable recording device worn at the subject's hip, and two thin elastic sensor insoles that were inserted at the foot-shoe or foot-brace interface. Several insole sizes are available and all subjects were individually fitted to ensure that the insole sensor fit completely inside the shoe in both conditions. The primary foot pressure variable of interest was the peak pressure corresponding to push off at the anatomical region of the hallux (big toe).
All sensors were individually calibrated using the Trublu ® calibration device (Novel Electronics Inc., St Paul, MN, USA). All data were collected at 100 Hz and analyzed using the Pedar ® -x Expert software and Novel Industry Professional software. Reported measurement error in the range of interest (50-500 kPa or 7.25-72.5 PSI) is 0.6% to 2.7% (11,12).
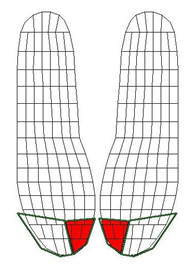
Analysis was performed by computing averages over approximately seven complete gait cycles for each subject and for each condition (with and without AFO) (5 trials x 2 conditions). An outline of the instrumented insole showing sensor locations is shown in Figure 1. The red area indicates the sensor mask used to compute peak pressures in this evaluation of push off.
RESULTS
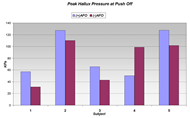
Hallux pressure during push off shows a significant trend towards higher values after the AFO was donned for four out of the five subjects tested. Pressures measured during push off are shown in Figure 2 for both AFO conditions. Higher push off pressures reflect an increase in propulsive force. This is necessary to increase step length and gait velocity; ultimately leading to increased efficiency during gait. However, one subject showed the opposite trend. Proper AFO fit was not assessed prior to data collection, so it may be possible that this individual's AFO was not properly fitted.
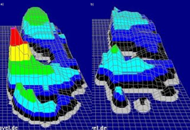
Pedobarography data are shown for one subject; warmer colors and 3D elevation indicate higher pressures. Figure 3 shows a summary plot of maximum foot pressures at all points on the foot. The (+)AFO condition is shown on the left; (-)AFO on the right. The maximum pressure at the Hallux is shown in both conditions, and verified to be the correct pressure during push off.
DISCUSSION/CONCLUSION
With this limited population, we have seen that the addition of an AFO to hemiplegic gait may cause a more efficient gait pattern by shifting pressure to the hallux during terminal stance for a more effective push off. These results suggest that Pedobarography may be a valuable outcome measure in determining the effectiveness of a prescribed AFO in hemiplegic gait.
Future work will focus on specific pressure areas to quantify improvements in gait with AFOs, and to identify potential areas of discomfort and malalignment before skin breakdown occurs. Ultimately, we hope to explore if dynamic pedobarography can enhance clinical observations and provide a more technical method of brace prescription, fitting and modification based on dynamic objective information acquired during normal walking.
REFERENCES
- American Heart Association. (2005). Heart disease and stroke statistics - 2005 update. Dallas, Texas: American Heart Association.
- Kelly-Hayes, M., Beiser, A., Kase, C. S., Scaramucci, A., D'Agostino, R. B., & Wolf, P. A. (2003). The influence of gender and age on disability following ischemic stroke: The framingham study. Journal of Stroke and Cerebrovascular Diseases, 12(3), 119-126.
- Gok, H., Kucukdeveci, A., Altinkaynak, H., Yavuzer, G., & Ergin, S. (2003). Effects of ankle-foot orthoses on hemiparetic gait. Clin Rehabil, 17(2), 137-139.
- Mojica, J. A., Nakamura, R., Kobayashi, T., Handa, T., Morohashi, I., & Watanabe, S. (1988). Effect of ankle-foot orthosis (afo) on body sway and walking capacity of hemiparetic stroke patients. Tohoku J Exp Med, 156(4), 395-401.
- Lehmann, J. F., Condon, S. M., Price, R., & deLateur, B. J. (1987). Gait abnormalities in hemiplegia: Their correction by ankle-foot orthoses. Arch Phys Med Rehabil, 68(11), 763-771.
- Lehmann, J. F., Condon, S. M., de Lateur, B. J., & Price, R. (1986). Gait abnormalities in peroneal nerve paralysis and their corrections by orthoses: A biomechanical study. Arch Phys Med Rehabil, 67(6), 380-386.
- Tyson, S. F., & Thornton, H. A. (2001). The effect of a hinged ankle foot orthosis on hemiplegic gait: Objective measures and users' opinions. Clin Rehabil, 15(1), 53-58.
- Lehmann, J. F., Esselman, P. C., Ko, M. J., Smith, J. C., deLateur, B. J., & Dralle, A. J. (1983). Plastic ankle-foot orthoses: Evaluation of function. Arch Phys Med Rehabil, 64(9), 402-407.
- Meyring, S., Diehl, R. R., Milani, T. L., Hennig, E. M., & Berlit, P. (1997). Dynamic plantar pressure distribution measurements in hemiparetic patients. Clin Biomech (Bristol, Avon), 12(1), 60-65.
- Orlin, M. N., & McPoil, T. G. (2000). Plantar pressure assessment. Phys Ther, 80(4), 399-409.
- Hsiao, H., Guan, J., & Weatherly, M. (2002). Accuracy and precision of two in-shoe pressure measurement systems. Ergonomics, 45(8), 537-555.
- Bray, L., Hillstrom, H., & Song, J. (2004). Accuracy of the novel pedar system. Gait and Posture, 12(2).
ACKNOWLEDGEMENTS
This material was based on work supported by the National Institute for Disability Rehabilitation Research (NIDRR) (H133P020012), Health Resources and Services Administration of the US Department of Health and Human Services, the University of Medicine and Dentistry of New Jersey, and the Henry H. Kessler Foundation. We would also like to thank Maria T. Schultheis, Ph.D. of the Psychology Department of Drexel University.
Author Contact Information:
Karen J. Nolan, Ph.D.
Kessler Medical Rehabilitation Research and Education Corporation
1199 Pleasant Valley Way
West Orange, NJ 07052, Phone (973) 324-3544
EMAIL: knolan@kmrrec.org
This should be in the right column.