Wrist Joint Reaction Moments in Children with Cerebral Palsy using Anterior and Posterior Walkers
Katherine Konop, BS1 , Kelly Strifling, PhD1 *, Mei Wang, PhD1 , Kevin Cao, MS1 , Jeffrey Ackman, MD2 , Jeffrey Schwab, MD3 and Gerald Harris, PhD, PE1,2,3
1 Orthopaedic and Rehabilitation Engineering Center, Milwaukee, WI
2 Shriners Hospitals for Children, Chicago, IL
3 Medical College of Wisconsin, Milwaukee, WI
*Corresponding author
ABSTRACT
Upper extremity (UE) joint kinetics during aided ambulation are not well characterized in the current literature. Biped UE joints are not anatomically designed to bear weight. To better understand the biomechanical implications of UE weight bearing, and to prescribe more effective methods for treatment and therapy, it is important to quantify UE kinetics during assisted gait. To address this challenge, an UE model that incorporates both kinematics and kinetics was developed for use with instrumented walkers. Three-dimensional wrist joint reaction moments are calculated for five children with cerebral palsy using both anterior and posterior walkers. The results indicate that, while there were no statistically significant differences, extension moments for both wrists, as well as the dynamic range of all three moments, tend to be greater with posterior walker use. Flexion moments were greater with anterior walker use. These findings could influence gait training routines, walker prescription strategies, and walker design.
Keywords:
Walker; Kinetics; Gait; Cerebral Palsy; Upper Extremity
BACKGROUND
Cerebral palsy (CP) is a neurological disorder resulting from pathologic brain development or injury. This disorder affects 2-3 babies per 1000 live births in the United States (1). Many cases of CP are characterized as spastic diplegic CP in which a velocity-dependent increase in muscle tone affects the lower limbs more severely than the uppers. Because of this, many children with CP require mobility aids, including anterior and posterior walkers, for stability.
The wrist is a complex joint, consisting of several small bones and articulations. For the purposes of this study, the wrist joint is simplified to allow rotation about two axes: flexion/extension and radial/ulnar deviation. However, this does not restrict the kinetics at the wrist. Three joint reaction moments are included in the model and kinetic analysis.
It is important to study the UE kinetics during walker usage because of the increased magnitude and repetition of UE loads (2,3,4). Some studies have examined the UE kinetics in Lofstrand crutch use (4,5). Others have looked at overall walker forces (6,7,8); however, the individual UE kinetics cannot be extracted from their data.
Some studies have compared anterior and posterior walker use in terms of energy expenditure and gait temporal and stride parameters (9,10). Our group recently published findings comparing upper extremity kinematics between the two walker types (11). The UE kinetics have not been reported for children with spastic diplegic CP using anterior and posterior walkers.
METHODS
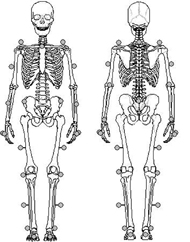
Five children (2 males, 3 females; aged 13.2±4.3 years) with spastic diplegic CP who routinely used posterior walkers were analyzed after IRB approval and informed consent were obtained. The average height was 134.3±6.6 cm and the average weight was 37.4±13.2 kg. Reflective surface markers were applied to the upper and lower extremities. The lower extremity (LE) marker set included fifteen 25-mm markers applied to the anatomical landmarks used in the traditional Plug-in-Gait model. The UE marker set included eighteen 16-mm reflective markers applied to the following anatomical landmarks: left and right anterior superior iliac spines (ASIS), sternal notch, vertebra C7, left and right acromion processes, mid-humeri, olecranon, mid-radii, ulnar styloid processes, and the third and fifth metacarpals (Figure 1). Markers were also placed on one front and one rear walker leg. Each subject underwent gait analysis, with motion data collected at 60 Hz using a 12-camera Vicon motion analysis system (Oxford Metrics, Oxford, UK). Kinetic data was collected at 1500 Hz using two specially designed walker handles (AMTI, Watertown, MA), each instrumented with a 6-axis strain gage-based load cell to measure three forces and three moments acting at the hand. After an acclimation period of at least 30 days, the same testing procedure was performed using the anterior walker.
The raw data was filtered with a Woltering filter and exported to an ASCII file. A custom UE kinematic and kinetic model was applied to the data to obtain joint angles, angular velocities and accelerations, as well as net joint reaction forces and moments. The kinetic model used body segment parameters, joint kinematics, and load cell data as inputs to an inverse dynamics model, which calculated the joint reaction forces and moments. Data was normalized to the product of body weight and stature (Nmm) to obtain a unitless metric. Data was time-normalized to 100% gait cycle. Paired comparisons were performed between the anterior and posterior walker by hand dominance (4 right-hand dominant, 1 left-hand dominant). Statistical analyses were done via the non-parametric Wilcoxon signed rank test with significance defined as a p-value less than 0.05.
RESULTS
Moments about the distal segment x-axis are termed medial/lateral moments, with medial being positive; moments about the y-axis are termed extension/flexion, with extension being positive; and moments about the z-axis are termed internal/external rotation, with internal rotation being positive. There were no statistically significant (p<0.05) differences between the two walker types. However, the peak wrist extension moment (resisting flexion) for both wrists tended to be greater with posterior walker use. The peak flexion moment (resisting extension) for the dominant wrist tended to be greater (more negative) with anterior walker use (p=0.0625). The dynamic range of all three of the moments also tended to be greater with posterior walker use (p=0.0625). These results are summarized in Table 1.
DISCUSSION/CONCLUSION
Walking aids function by relieving the lower extremities of the loading experienced in normal gait. These loads are transferred to the upper extremities. Since the upper extremities do not normally experience loads of this magnitude and repetition, it is important to quantify the loads and the UE joint kinetics. A primary biomechanical concern is that the wrist joint, with its many small bones and ligaments, may be vulnerable to overuse injury with extended use of a walker.
This study has shown that posterior walker use tended to subject the wrist joints to greater loading when compared to the anterior walker. While the results of the current study are based on a relatively small population, continued findings of this nature could be helpful in considering which walker to prescribe to a specific patient. The results from this study support the continued and expanded study of a larger population of walker users and an expanded analysis to include the full set of UE joint kinetics.
REFERENCES
- Odding, E., Roebroeck, M., & Stam, H. (2006). The epidemiology of cerebral palsy: incidence, impairments and risk factors. Disability and Rehabilitation, 28(4):183–191.
- Haubert, L., Gutierrez, D., Newsam, C., Gronley, J., Mulroy, S., & Perry, J. (2006). A comparison of shoulder joint forces during ambulation with crutches versus a walker in persons with incomplete spinal cord injury. Archives of Physical Medicine and Rehabilitation, 87(1):63–70.
- Melis, E., Torres-Moreno, R., Barbeau, H., & Lemaire, E. (1999). Analysis of assisted gait characteristics in persons with incomplete spinal cord injury. Spinal Cord, 37(6):430–439.
- Requejo, P., Wahl, D., Bontrager, E., Newsam, C., Gronley, J., Mulroy, S., Perry, J. (2005). Upper extremity kinetics during Lofstrand crutch-assisted gait. Medical Engineering and Physics, 27, 19-29.
- Slavens, B., Frantz, J., Sturm, P., Harris, G. (2007). Upper extremity dynamics during Lofstrand crutch-assisted gait in children with myelomeningocele. Journal of Spinal Cord Medicine, 30: 77-83.
- Fast, A., Wang, F., Adrezin, R., Cordaro, M., Ramis, J. (1995). The instrumented walker: Usage patterns and forces. Archives of Physical Medicine and Rehabilitation, 76: 484-491.
- Opila, K., Nicol, A., & Paul, J. (1987). Upper limb loadings of gait with crutches. Journal of Biomechanical Engineering, 109(4):285–290.
- Pardo, R., Deathe, A., Winter D. (1993). Walker user risk index: A method for quantifying stability in walker users. American Journal of Physical Medicine and Rehabilitation, 72(5): 301-305.
- Mattsson, E., Anderson, C. (1997). Oxygen cost, walking speed, and perceived exertion in children with cerebral palsy when walking with anterior and posterior walkers. Developmental Medicine and Child Neurology, 39: 671-676.
- Park, E., Park, C., Kim, J. (2001). Comparison of anterior and posterior walkers with respect to gait parameters and energy expenditure of children with spastic diplegic cerebral palsy. Yonsei Medical Journal, 42(2): 180-184.
- Strifling, K., Lu, N., Wang, M., Cao, K., Ackman, J., Klein, J., Schwab, J., Harris, G. (2008). Comparison of upper extremity kinematics in children with spastic diplegic cerebral palsy using anterior and posterior walkers. Gait and Posture, in press.
ACKNOWLEDGEMENTS
This project is supported by NIDRR grant H133G010069 and the Orthopaedic and Rehabilitation Engineering Center (OREC) – Marquette University / Medical College of Wisconsin.
*Author Contact Information:
Kelly Strifling, PhD, Marquette University
Academic Support Facility Rm. 105—OREC
735 N. 17th St.
Milwaukee, WI 53233
PHONE: 414-288-6003
EMAIL: kelly.strifling@marquette.edu