Thais Pousada*, Javier Pereira*, Laura Nieto*, Betania Groba*, Emiliano Díez**
*Universidade da Coruña; ** Universidad de Salamanca (Spain)Introduction
Neuromuscular disorders (NMD) are a group of diseases which have in common their high heterogeneity in incidence, hereditary, aetiology, prognosis and functional impairments.(Cup et al., 2007; Fowler, Graves, Wetzel, & Spencer, 2004) Although the degree and severity can vary, the main characteristic of all of the above neuromuscular diseases is the progressive clinical course, characterized by a decrease in muscle strength, as well as limb contractures, spine deformity and decreased pulmonary function.(Pieterse et al., 2008)
Despite the fact they are still able to walk, the risk of falls and the presence of fatigue in activities with high mobility demands lead to the need to receive an assistive technology (AT). Furthermore, the wheelchair may be necessary as a device to enhance the patient’s level of mobility and functional ability and to reduce the dependence from the caregiver.(Stein J & Cassell J, 2007)
The psychosocial impact associated with the use of a wheelchair is an important aspect which determines its integration into the daily life of the user(Salminen, Brandt, Samuelsson, Toytari, & Malmivaara, 2009). Thus, an evaluation of the effect on quality of life as outcome measure is important in order to optimize the process of prescribing and providing this AT.(De Ruyter F, 1997)
Research question
Two were the main objectives of this study: (1) to determine the psychosocial impact (positive or negative) that wheelchair has on the Quality of life (QoL) of people with NMD; (2) to determine if psychosocial impact of wheelchair is influenced by contextual factors.
METHOD
Sample
The study was done with a sample of sixty persons with NMD, users of wheelchair and living in Galicia (Spain). Men were 36 and women were 24, the mean of age was 35.15, and the 80% was single and the 20% was married. The main diagnosis was Muscular Dystrophy (35), followed by Spinal Muscular Amyotrophic (7).
Study Design
A cross-sectional study has been used. This methodology involves mostly observation, it is a descriptive study. This study lasted 16 months, starting from January 15, 2010 until May 15, 2011.
Variables and tools
The main factor studied in this work has been the impact on the quality of life (in terms of psychosocial constructs of competence, adaptability and self-esteem). Moreover, different variables have been chosen and defined with the aim of collecting the necessary data for the analysis and subsequent determination of results.
To get the data, several assessment tools were used:
Psychosocial Impact Assistive Device Scale (PIADS): It is a 26-item self-rating scale designed to measure the impact of assistive technology (AT) on the QoL of the user of these devices. Dimensions of PIADS are summarized in three domains: adaptability, competence and self-esteem. Scores can range from -3 (maximum negative impact) to +3 (Maximum positive impact).(Jutai J & Day H, 2002; J. Jutai, Rigby, Ryan, & Stickel, 2000)
Functional Independence Measure (FIM): The FIM is the most widely accepted and used in assessing the outcomes of rehabilitation interventions. The FIM is a measurement of user’s capacity, not of the deficit, so FIM is based on a medical model of assessment that places importance on cure.Smith1996 The questionnaire assesses six areas of function across 18 items: self-care, sphincter control, mobility, locomotion, communication and social cognition. Those areas are grouped into two domains: Motor (13 items) and Cognitive (5 items). Each item is scored using the Linker seven-point scale from 1 (total assistance is needed) to 7 (total independence).(Uniform Data System for Medical Rehabilitation, 1997)
Specific Design questionnaire: It was created by research group. It is divided into two sections: the first one collects data from variables related to the person and the description of carrying out and participating in activities, and about to the environment’s characteristics (User questionnaire); the second one includes information involving the features of the wheelchair used (Wheelchair data sheet).
Procedure
The specific questionnaire, PIADS and FIM were administrated in a semi-structured interview (39 cases) and 21 clients completed them themselves. Ethical criteria of Spanish Health Institutions were respected.
Statistical analyses were performed using non-parametric test (U Mann Whitney, Kruskal Wallis and Spearman Correlations) on Spss v.16 for Windows®. Only those results which were statistically significant (p<0.05) are reported in this text.
Results
Descriptive Data:
The mean age of participants was 35.15 (SD = 17.1), the largest age range being between 36 and 50 years old (n = 18). Regarding clinical aspects, the NMD diagnoses were heterogeneous. However, the muscular dystrophy (MD) group was the largest one (58.3%). Most of those who are independent in terms of locomotion (assessed using the Locomotion FIM) use electric wheelchairs (n = 26) and can be classified as people with non-functional ambulation (n = 31), according to Hoffer’s classification.(Hoffer, Feiwell, Perry, Perry, & Bonnett, 1973)
Powered wheelchairs were used by 31 persons, 23 cases used manual wheelchair (self-propulsed) and the last 6 needed the support of caregiver to propel the device. Regarding the usage of the wheelchair, it is worth highlighting the width of the year range during the user’s life (36 years), which goes from 1 (minimum) to 37 years (maximum).
Psychosocial Impact of using a wheelchair
Table 1 shows the results from PIADS, where the psychosocial impact of wheelchair was moderately positive on participants. Adaptability was the dimension with higher score (M=1.23), while self-esteem scores were significantly lower in the three types of devices (M=0.92). Overall, these findings suggest that reported impacts were greater in domains associated with perceived capability and attitude toward participation.
Type of Wheelchair |
Dimensions of PIADS |
||
|---|---|---|---|
Competence Mean (SD) |
Adaptability Mean (SD) |
Self-Esteem Mean (SD) |
|
Electric Wheelchair (n=31) |
1.412 (0.87) |
1.6 (1.07) |
1.12 (0.91) |
Manual Wheelchair (Self-propulsed) (n=23) |
0.72 (0.59) |
0.94 (0.95) |
0.72 (0.82) |
Manual Wheelchair (not self-propulsed) (n=6) |
0.49 (0.71) |
0.45 (0.41) |
0.65 (0.76) |
Total sample (N=60) |
1.06 (0.83) |
1.23 (1.04) |
0.92 (0.87) |
Influence of factors on the impact of the wheelchair
In order to know the influence of several factors, as demographic and clinical data or level of independence, bivariate analyses were applied.
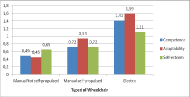
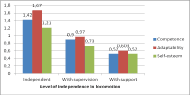
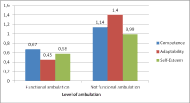
The factors with strongest influence on psychosocial impact are showed in Figure 1, 2 and 3. Powered wheelchair (p<0.01) and the higher independence in Locomotion (p<0.01) have a positive effect on perceived impact derived of wheelchair’s use on quality of life. , not having functional ambulation (according to Hoffer’s classification)(Hoffer et al., 1973) has also an influence on the impact of wheelchair, especially in terms of adaptability.
Regarding the variables related to personal characteristics, diagnostic conditions seem to have a positive influence on the impact that wheelchair has on quality of life. Thus, having been diagnosed with arthrogryposis (competence=1.98; adaptability=1.55; self-esteem=1.22) at an early age (in terms of self-esteem, r=-0.270; p<0.05) leads to a more positive impact.
Regarding the analysis of the influence of environmental factors, the only remarkable difference was related to the place of residence. The mean score for the self-esteem subscale is significantly lower (p<0.05) for those who lived in a dwelling compared to those who lived in a care facility or residential care facility.
The influence of social environment becomes more evident since the psychosocial impact seems to be influenced by the type of caregiver (relative or professional) in competence (p<0.05), adaptability (p<0.05) and self-esteem (p<0.05). That is, having a professional caregiver increases positively the impact of wheelchair on subjective well-being.
Discussion
Results from the application of PIADS demonstrate that wheelchairs appear to have a positive impact on the perceived quality of life of persons with NMD. Across the three PIADS subscales, the mean scores are similar to previous studies, for example, in persons with Muscular Sclerosis (Demers, Weiss-Lambrou, & Ska, 1996) or Amyotrophic Lateral Sclerosis.(Devitt R, Chau B, & Jutai JW, 2003; J. Jutai & Gryfe, 1998)
The obtained data indicate that powered wheelchair offers improved competence and adaptability for users. Moreover, independence in personal mobility is the main factor determining a positive effect. Nevertheless, the impact of wheelchair on quality of life is hardly affected by functional ambulation and/or low level of use.
This way, the wheelchair becomes an additional part of the person affected with NMD. Consideration is given to a fundamental, environmental factor to maintain independence in activities as basic as mobility. The feeling of freedom to get around, given by the wheelchair itself, contributes to perceived well-being, to self-esteem and to self-confidence, to the desire of trying new things and to the ability to take advantage of opportunities, as well as to the feeling of competence and efficiency.(Devitt R et al., 2003)(Devitt R et al., 2003)
Results also show that there is a clear difference in terms of independence regarding activities of daily living between participants who use their wheelchair to carry them out and those who don’t. However, the mean scores of PIADS are not significantly different between both groups of users
In this study, no significant differences have been found for the scores of competence and adaptability in relation to the presence of adaptations and/or architectural barriers. Nevertheless, architectural barriers are a limiting environmental factor in the use of wheelchairs. Modification of the user’s home is necessary in order for users with NMD to facilitate the usage of this assistive device.
Social context has had a greater influence on the impact perceived and derived from the wheelchair than the physical environment. Hence, the support of people seems to be more significant than environmental barriers.
As the wheelchair is a fundamental environmental factor to maintain independence in different activities, it is important to apply tools like PIADS on clinical practice. Like this, the determination of effects of wheelchair use and the factors that shed light on the impacts of such usage will be facilitate. It could assume that during the process of prescribing a wheelchair, the professional health care provider should consider not only the user but also his/her needs in terms of goals, fulfilment of activities, and degree of participation, as well as his/her interaction with the environment.References
Cup, E. H., Pieterse, A. J., Knuijt, S., Hendricks, H. T., van Engelen, B. G., Oostendorp, R. A., et al. (2007). Referral of patients with neuromuscular disease to occupational therapy, physical therapy and speech therapy: Usual practice versus multidisciplinary advice. Disability and Rehabilitation, 29(9), 717-726.
De Ruyter F. (1997). The importance of outcome measures for assistive tehcnology service delivery systems. Technol Disabil, 6, 89-104.
Demers, L., Weiss-Lambrou, R., & Ska, B. (1996). Development of the quebec user evaluation of satisfaction with assistive technology (QUEST). Assistive Technology : The Official Journal of RESNA, 8(1), 3-13.
Devitt R, Chau B, & Jutai JW. (2003). The effect of wheelchair use on the quality of life of persons with multiple sclerosis. Occupational Therapy in Health Care, 17(3/4), 63-79.
Fowler, E. G., Graves, M. C., Wetzel, G. T., & Spencer, M. J. (2004). Pilot trial of albuterol in duchenne and becker muscular dystrophy. Neurology, 62(6), 1006-1008.
Hoffer, M. M., Feiwell, E., Perry, R., Perry, J., & Bonnett, C. (1973). Functional ambulation in patients with myelomeningocele. The Journal of Bone and Joint Surgery.American Volume, 55(1), 137-148.
Jutai J, & Day H. (2002). Psychosocial impact of assistive devices scale (PIADS© ). Technology & Disability, 14, 107-111.
Jutai, J., & Gryfe, P. (1998). Psychological factors in the assessment of assistive technologies. Proceedings of RESNA ‘98, pp. 54-65.
Jutai, J., Rigby, P., Ryan, S., & Stickel, S. (2000). Psychosocial impact of electronic aids to daily living. Assistive Technology : The Official Journal of RESNA, 12(2), 123-131.
Pieterse, A. J., Cup, E. H., Knuijt, S., Hendricks, H. T., van Engelen, B. G., van der Wilt, G. J., et al. (2008). Development of a tool to guide referral of patients with neuromuscular disorders to allied health services. part one. Disability and Rehabilitation, 30(11), 855-862.
Salminen, A. L., Brandt, A., Samuelsson, K., Toytari, O., & Malmivaara, A. (2009). Mobility devices to promote activity and participation: A systematic review. Journal of Rehabilitation Medicine : Official Journal of the UEMS European Board of Physical and Rehabilitation Medicine, 41(9), 697-706.
Stein J, & Cassell J. (2007). An introductory guide for families with a child newly diagnosed with neuromuscular dystrophy or an associated neuromuscular condition (1st ed.). London: Muscular Dystrophy Campain.
Uniform Data System for Medical Rehabilitation. (1997). Functional independence measure, version 5.1. New York: Buffalo General Hospital.
Acknowledgements
This study was funded, in part, by the Professional Occupational Therapist College of Extremadura (COPTOEX).