Martine Blouin a,c, Mathieu Lalumière b, Dany Gagnon b, Félix Chénier a,c and Rachid Aissaoui a,c
a Laboratoire de Recherche en Imagerie et Orthopédie, Centre de Recherche du CHUM, Montréal, QC, Canada; b École de Réadaptation, Université de Montréal, QC, Canada; c Department of Automated Manufacturing Engineering, École de Technologie Supérieure, Montréal, QC, CanadaABSTRACT
This study describes a new simulator that provides haptic biofeedback to help manual wheelchair users gain a more effective propulsion pattern. Propulsion effectiveness is measured using the mechanical effective force (MEF). The simulator implements a dynamic model that replicates overground propulsion conditions. Haptic biofeedback increases the feeling of rolling resistance if the user’s MEF pattern deviates from a chosen target MEF pattern. Six manual wheelchair users participated in a training session on the simulator with haptic biofeedback. On average, participants increased their mean MEF by 6.3% on the left side and 7.5% on the right side during the training session compared to the pre-training period. Moreover, participants generally succeeded to follow the target pattern during training. Haptic biofeedback appears to improve propulsion effectiveness in manual wheelchair users.
BACKGROUND
Manual wheelchair propulsion is a functional activity associated with a high prevalence of shoulder muscles impairments (Paralyzed Veterans of America Consortium for Spinal Cord Medicine [PVACSCM], 2005). Shoulder muscles impairments make activities of daily living harder to perform and compromise functional mobility (PVACSCM, 2005). A more effective propulsion pattern could allow manual wheelchair users (MWUs) to reduce the amount of force they require to move their wheelchair at a given speed, which could in turn decrease their risk of developing secondary shoulder muscles impairments (de Groot, Veeger, Hollander & van der Woude, 2002).
Propulsion effectiveness is often measured using the mechanical effective force (MEF), a squared ratio between the tangential and the total forces applied on the handrims. A few research groups have attempted to increase MEF through training sessions among healthy individuals or MWUs, with contradictory results (de Groot et al., 2002; Kotajarvi, Basford, An, Morrow & Kaufman, 2006). Kotajarvi et al. (2006) concluded that the visual feedback they provided during their training might not have been optimal to improve propulsion effectiveness in their study group of experienced MWUs.
Our team recently developed a wheelchair simulator that provides real-time haptic biofeedback (HB) on MEF along the push phase (Chénier, Bigras & Aissaoui, 2013). HB uses the sense of touch, including the perception of forces and movements, to provide information to an end user. By its kinetic nature, we believe that HB represents a preferred form of feedback to stimulate the acquisition of new motor skills required for more effective propulsion.
PURPOSE
The purpose of this study is two-fold: (1) to investigate whether HB can bring MWUs to increase their MEF and follow a chosen target MEF pattern during a single training session on the simulator, and (2) to test the simulator with experienced MWUs to identify directions for future improvements.
DESCRIPTION OF THE SIMULATOR
The simulator, shown in schematic form in Figure 1, includes two instrumented wheels (SmartWheel, Three Rivers Holdings, LLC) that measure the forces and moments applied on the handrims. It also includes a computer that runs a real-time operating system (xPC Target, The Mathworks Inc.), and two motors (Kollmorgen) attached to rollers that independently drive the two wheels at the correct velocities (Chénier et al., 2013). The simulator implements a unique wheelchair-user dynamic model that depends on three parameters: the mass m of the wheelchair-user system, its moment of inertia Io and a rolling resistance Froll defined for a certain type of floor (Chénier, Bigras & Aissaoui, 2011).
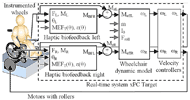 Figure 1 : Schematic of the simulator and its operation. d
Figure 1 : Schematic of the simulator and its operation. dWhen the HB is disabled, the left and right propulsive moments generated by the user (MzL and MzR) are directly fed to the dynamic model. However, when the HB is enabled, active biofeedback moments MBFL and MBFR are subtracted from MzL and MzR. The differences MzL – MBFL and MzR – MBFR become the input for the dynamic model. As MBF increases, so does the apparent rolling resistance, because the user needs to generate extra propulsive moments Mz = MBF to keep the same velocity. On the contrary, if the user follows exactly the target MEFT, zero biofeedback moments is generated.
We believe that MWUs will be able to modify their MEF patterns towards MEFT by searching for the propulsion pattern with the lowest resistance. MBF moments are calculated in function of the relative hand position (θ), for each side separately, using equation 1:
| M |
(1) |
where:
|
MEF = (MZ/R)2/Fx2 +Fy2 + Fz2 |
(2) |
and where:
- ε is the chosen biofeedback intensity modulator;
- MEF
 T is the chosen target MEF pattern;
T is the chosen target MEF pattern; - F
 i and M
i and M i are the forces and moments applied by the user on axis i in Newtons and Newtons-meters, x being the anteroposterior axis, y being the vertical axis, and z being the mediolateral axis;
i are the forces and moments applied by the user on axis i in Newtons and Newtons-meters, x being the anteroposterior axis, y being the vertical axis, and z being the mediolateral axis; - R is the handrim radius in meters.
EXPERIMENTAL PROTOCOL
Participants
Six MWUs (age: 45 ± 12 years; weight: 82 ± 15 kg) with spinal cord injury (lesion level: T2-T12; time since injury: 15 ± 9 years) participated in this study. The study was approved by the research ethics committees of the École de Technologie Supérieure and the Centre for Interdisciplinary Research in Rehabilitation of Greater Montreal. Participants were included if they used a manual wheelchair as a primary means of mobility, could perform wheelchair-to-wheelchair transfers independently, and reported no sign of pain that could have hindered their propulsion biomechanics.
Preparation
Participants were weighed with their own wheelchair using an adapted scale (Health-o-meter, Balance Bourbeau Inc.). The wheelchair’s weight was also recorded separately. Participants were assisted to transfer to the wheelchair mounted on the simulator. The simulator’s parameters m, I0 and Froll were adjusted as follows: m was set to the participant’s mass with his personal wheelchair, I![]() 0 was fixed to the average moment of inertia found by Chénier et al. (2011) for 10 participants, and F
0 was fixed to the average moment of inertia found by Chénier et al. (2011) for 10 participants, and F![]() roll was computed using F
roll was computed using F![]() roll = μ•m•g, with μ being the average rolling resistance coefficient of 0.0138 reported by Chénier et al. (2011) and g being the gravity constant 9.81 m/s
roll = μ•m•g, with μ being the average rolling resistance coefficient of 0.0138 reported by Chénier et al. (2011) and g being the gravity constant 9.81 m/s![]() 2.
2.
Pre-training
Participants propelled on the simulator at a self-selected comfortable speed for three one-minute trials (one familiarization trial and two experimental trials). Force and moment data were recorded bilaterally at 240 Hz using the SmartWheels during the last 30 seconds of each experimental trial. Patterns of MEF expressed as a function of time (MEF(t)) were calculated using equation 2 for each push. MEF(t) patterns were then normalized between 0% and 100% of the push phase to get MEF(%push) patterns.
The 10 most repeatable pushes of each trial were selected using a method based on Kadaba et al. (1989). The pushes were then averaged to create the mean MEF pattern achieved during pre-training (MEF![]() ini(%push)). The mean push angle (PA
ini(%push)). The mean push angle (PA![]() ini), expressed in degrees, was also calculated from the same pushes.
ini), expressed in degrees, was also calculated from the same pushes.
Haptic biofeedback definition
The target MEF![]() T(%push) was defined using MEF
T(%push) was defined using MEF![]() ini(%push) as a starting point. MEF
ini(%push) as a starting point. MEF![]() T(%push)’s maximum was set to MEF
T(%push)’s maximum was set to MEF![]() ini(%push)’s maximum plus 10%. Furthermore, MEFT(%push) was set equal to MEF
ini(%push)’s maximum plus 10%. Furthermore, MEFT(%push) was set equal to MEF![]() ini(%push) between 0%-10% and 90%-100% of the normalized push phase. Between 10%-90%, MEFT(%push) was generated using two half-Gaussian functions, the first defined between MEF
ini(%push) between 0%-10% and 90%-100% of the normalized push phase. Between 10%-90%, MEFT(%push) was generated using two half-Gaussian functions, the first defined between MEF![]() T(10%) and max(MEF
T(10%) and max(MEF![]() T), and the second defined between max(MEF
T), and the second defined between max(MEF![]() T) and MEF
T) and MEF![]() T(90%). MEF
T(90%). MEF![]() T(%push) was then expressed as MEF
T(%push) was then expressed as MEF![]() T(θ), with 0%=0 degree and 100%=PA
T(θ), with 0%=0 degree and 100%=PA![]() ini.
ini.
The biofeedback intensity modulator ε(%push) was set proportional to each participant’s mean pre-training mediolateral moment (Mz![]() ini(%push)). No biofeedback was provided in the early-beginning and late-end portions of the push phase (ε(%push) set to zero) because these are regions of unstable contact between the hands and wheels. Parameter ε(%push) was then expressed as ε(θ) with the same methodology as for MEF
ini(%push)). No biofeedback was provided in the early-beginning and late-end portions of the push phase (ε(%push) set to zero) because these are regions of unstable contact between the hands and wheels. Parameter ε(%push) was then expressed as ε(θ) with the same methodology as for MEF![]() T(θ).
T(θ).
Training
Four three-minute trials (three familiarization trials and one experimental trial) with HB were conducted. HB started 3 seconds after the beginning of the trial and was kept active until the end. Participants were instructed to strive for the lowest resistance possible. During the last 30 seconds of the experimental trial, handrim force and moment data were recorded.
Closure
Participants were asked to comment subjectively on the experiment and on their appreciation of the simulator.
Post-experiment data analysis
Force and moment data were filtered using an 8th order Butterworth low-pass filter with a 30 Hz cutoff frequency. The 10 most repeatable pushes of each of the pre-training and training trials were identified. MEF patterns were normalized as described before. The middle portion (25%-75%) of each normalized pattern was selected for the analysis because most of the propulsion effort is provided there. The average MEF value in each push () and the root-mean-square deviation between the achieved MEF pattern and MEF![]() T in each push (ΔMEF
T in each push (ΔMEF![]() RMS) were computed between 25%-75%. An increase in meant that propulsion effectiveness was improved. A decrease in ΔMEF
RMS) were computed between 25%-75%. An increase in meant that propulsion effectiveness was improved. A decrease in ΔMEF![]() RMS meant that the participants’ achieved MEF pattern followed the target better. and ΔMEF
RMS meant that the participants’ achieved MEF pattern followed the target better. and ΔMEF![]() RMS values were averaged for each trial.
RMS values were averaged for each trial.
RESULTS
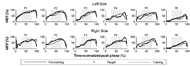 Figure 2 : Average MEF patterns achieved by participants during pre-training and training in comparison with the target MEFT on both sides. Patterns are normalized between 0% and 100% of the push phase. d
Figure 2 : Average MEF patterns achieved by participants during pre-training and training in comparison with the target MEFT on both sides. Patterns are normalized between 0% and 100% of the push phase. dFigure 2 shows participants’ average MEF patterns achieved during pre-training and training in comparison with MEF![]() T on both sides. Participants generally increased their MEF between the pre-training and the training in the middle portion of the push (light gray zone). On the left side, participants P2, P3, P5 and P6 succeeded to modify their MEF patterns during training to make it more similar to the target. All participants managed to do the same on the right side.
T on both sides. Participants generally increased their MEF between the pre-training and the training in the middle portion of the push (light gray zone). On the left side, participants P2, P3, P5 and P6 succeeded to modify their MEF patterns during training to make it more similar to the target. All participants managed to do the same on the right side.
Table 1 reports values of and ΔMEF![]() RMS. increased by an average of 6.3% on the left and 7.5% on the right side between pre-training and training. ΔMEF
RMS. increased by an average of 6.3% on the left and 7.5% on the right side between pre-training and training. ΔMEF![]() RMS decreased by an average of 2.4% on the left and 4.7% on the right side between the two same periods.
RMS decreased by an average of 2.4% on the left and 4.7% on the right side between the two same periods.
Participants enjoyed trying out the simulator and felt it could be useful in a clinical setting. Most of them mentioned they had some trouble understanding how exactly they needed to push the wheels in order to get the lowest resistance.
|
Participant |
P1 |
P2 |
P3 |
P4 |
P5 |
|---|---|---|---|---|---|---|
Left side |
Ini (%) |
75.0 |
63.3 |
52.9 |
42.3 |
48.6 |
Trn (%) |
74.3 |
72.2 |
65.9 |
42.6 |
58.6 |
|
Difference in (%) |
-0.7 |
8.9 |
13.0 |
0.3 |
10.0 |
|
ΔMEF |
9.3 |
18.8 |
13.1 |
14.9 |
20.9 |
|
ΔMEF |
10.6 |
15.7 |
11.1 |
17.3 |
14.0 |
|
Difference in ΔMEF |
1.3 |
-3.1 |
-2.0 |
2.4 |
-6.9 |
|
Right side |
Ini (%) |
56.1 |
56.0 |
46.0 |
50.7 |
43.4 |
Trn (%) |
61.5 |
72.3 |
53.3 |
57.9 |
49.7 |
|
Difference in (%) |
5.3 |
16.3 |
7.4 |
7.2 |
6.4 |
|
ΔMEF |
13.3 |
18.3 |
12.8 |
10.3 |
23.0 |
|
ΔMEF |
9.9 |
11.2 |
7.2 |
7.7 |
18.3 |
|
Difference in ΔMEF |
-3.5 |
-7.1 |
-5.7 |
-2.6 |
-4.7 |
DISCUSSION
The simulator from this study appears to be a useful tool for the development of training programs aiming at improving manual wheelchair propulsion. Propulsion effectiveness was increased during training when compared to pre-training (increase in ). Furthermore, most participants (especially P2, P3 and P6) were able to change their average MEF pattern between the pre-training and the training (Figure 2), and managed to follow the target better during training (decrease in ΔMEF![]() RMS). Although most participants mentioned they had some trouble intellectualizing the HB, they were able to react to it by modifying their propulsion pattern towards the target.
RMS). Although most participants mentioned they had some trouble intellectualizing the HB, they were able to react to it by modifying their propulsion pattern towards the target.
It is hard to compare this study with previous studies from de Groot et al. (2002) and Kotajarvi et al. (2006). These studies carried on their training on different ergometers and did not set up any targets or boundaries to guide the MEF increase throughout the push phase. Moreover, this is the first time HB is provided to MWUs during a propulsion task.
Study limitations
This study had a few limitations that should be acknowledged. For instance, participants were not propelling in their own wheelchair on the simulator, which could have modified their propulsion biomechanics (Yang, Koontz, Yeh & Chang, 2012). To minimize this error, each participant’s used his/her own seat cushion and backrest angle was adjusted as close as possible to that of the participant’s personal wheelchair. Furthermore, MEF was calculated based on an estimation of the tangential force, obtained from the propulsive moment around the wheel hub. Although this approximation has been used in many studies, it remains valid only if a negligible moment is produced by the hand around the mediolateral axis (Cooper, Robertson, VanSickle, Boninger & Shimada, 1997). This is usually the case for propulsion on flat surfaces (VanSickle, Cooper, Boninger, Robertson & Shimada, 1998).
CONCLUSION
This study provides a unique insight into a new simulator that provides real-time HB on propulsion effectiveness. The results show that MWUs are able to react to HB by modifying their propulsion pattern towards better effectiveness. The proposed training session will soon be incorporated into a more comprehensive wheelchair training program, while parameters MEFT and ε will be optimized. As for the simulator per se, it offers many exclusive features that will certainly help to carry out future research in the field.
REFERENCES
Chénier, F., Bigras, P., & Aissaoui, R. (2011). A new dynamic model of the manual wheelchair for straight and curvilinear propulsion. In Proceedings of the IEEE International Conference on Rehabilitation Robotics (ICORR) (pp. 1-5). Piscataway, NJ: Institute of Electrical and Electronics Engineers.
Chénier, F., Bigras, P., & Aissaoui, R. (2013). A new wheelchair ergometer designed as an admittance-controlled haptic robot. IEEE/ASME Transactions on Mechatronics, PP(99), 1-8. Retrieved November 1, 2013, from http://ieeexplore.ieee.org/xpl/articleDetails. jsp?arnumber=6408247.
Cooper, R.A., Robertson, R. N., VanSickle, D. P., Boninger, M. L., & Shimada, S. D. (1997). Methods for determining three-dimensional wheelchair pushrim forces and moments: a technical note. Journal of Rehabilitation Research & Development, 34(2), 162-170.
de Groot, S., Veeger, H.E., Hollander, A.P., & van der Woude, L.H. (2002). Consequence of feedback-based learning of an effective hand rim wheelchair force production on mechanical efficiency. Clinical Biomechanics, 17(3), 219-226.
Huang, V.S., & Krakauer, J.W. (2009). Robotic neurorehabilitation: a computational motor learning perspective. Journal of NeuroEngineering and Rehabilitation, 6(5). Retrieved November 11, 2013, from http://www.jneuroengrehab.com/content/6/1/5.
Kadaba, M.P., Ramakrishnan, H.K., Wootten, M.E., Gainey, J., Gorton, G., & Cochran, G.V. (1989). Repeatability of kinematic, kinetic, and electromyographic data in normal adult gait. Journal of Orthopaedic Research, 7(6), 849-860.
Kotajarvi, B.R., Basford, J.R., An, K.N., Morrow, D.A., & Kaufman, K.R. (2006). The Effect of Visual Biofeedback on the Propulsion Effectiveness of Experienced Wheelchair Users. Archives of Physical Medicine and Rehabilitation, 87(4), 510-515.
Paralyzed Veterans of America Consortium for Spinal Cord Medicine. (2005). Preservation of Upper Limb Function Following Spinal Cord Injury. Journal of Spinal Cord Medicine, 28(5), 434-470.
VanSickle, D.P., Cooper, R.A., Boninger, M.L., Robertson, R.N., & Shimada, S.D. (1998). A unified method for calculating the center of pressure during wheelchair propulsion. Annals of Biomedical Engineering, 26(2), 328-336.
Yang, Y.-S., Koontz, A.M., Yeh, S.-J., & Chang, J.-J. (2012). Effect of Backrest Height on Wheelchair Propulsion Biomechanics for Level and Uphill Conditions. Archives of Physical Medicine and Rehabilitation, 93(4), 654-659.
ACKNOWLEDGMENTS
The authors would like to thank all the participants who provided their time and energy to test this simulator. We also thank the Lindsay Rehabilitation Hospital Foundation, the SensoriMotor Rehabilitation Research Team, the Fonds de recherche du Québec - Nature et technologies, and the Natural Sciences and Engineering Research Council of Canada for funding this project.
Audio Version PDF Version