APPLICATION OF BODY WEIGHT SUPPORT SYSTEMS IN REAL WORLD SETTINGS ACROSS THE LIFESPAN
Devina S. Kumar1, Elena Kokkoni1, Samuel Logan2, Tracy Stoner3, James C. Galloway1,3
1Biomechanics and Movement Science, University of Delaware, Newark, DE
2Biological and Population Health Sciences, Oregon State University, Corvallis, OR
3Physical Therapy, University of Delaware, Newark, DE
BACKGROUND
Participation in real-world environments is challenging for patients with mobility impairments throughout lifespan. For children, opportunities for play and physical activity can be hampered by the limitations in ambulatory level (Wrotniak, Epstein, Dorn, Jones & Kondilis, 2006). Similarly, for adults with severe neurological conditions such as brain injury, community independence and employment opportunities are often diminished due to their long term impairments (Shames, Treger, Ring, & Giaquinto, 2007). Overall, mobility issues impact quality of life and participation in daily activities at both the individual and societal levels.
Clinic-based mobility interventions often involve body weight support systems (BWSSs) over treadmill and/or over ground (Cherng, Liu, Lau & Hong, 2007; Damiano & DeJong, 2009). The positive effects of clinic-based BWSSs on gait may not carryover to real life situations in which ambulation is coupled with multiple other tasks. The potential effects of daily use of BWSSs within community settings has not been previously examined and is the focus of this paper.
Our lab has co-designed a new generation of open area BWSSs for use within real life situations such as at home and at work. If feasible and effective, these innovative BWSSs could alter when and how mobility related interventions are provided for pediatric and adult populations.
PURPOSE
Current literature lacks the results of high dosage applications of body weight supported training in naturalistic settings. In this paper, we focus on two areas of interest:
1) Feasibility of BWSS use as reflected in the levels of i) implementation, ii) acceptability, iii) demand, iv) practicality, and v) adaptation.
2) Clinical outcomes related to BWSS use as reflected by measures of i) dynamic balance, ii) functional ambulation, and iii) submaximal endurance.
METHOD
Subjects:
Pediatric case: A 5-year old male subject, diagnosed with L4 to L5 myelomeningocele form of spina bifida at his birth at full-term. At study onset, the subject walked for short distances (100 feet) on level terrain using lofstrand crutches. He was unable to stand unsupported, but could stand at table top surfaces using his upper body for balance and/or support. He received physical therapy twice per week that focused on functional strength, standing balance, and gait training.
Adult cases: 2 female subjects (34 and 23 years of age) with a history of Traumatic Brain Injury (TBI). At study onset, both were unable to stand unsupported, required constant supervision. Both had attended various rehabilitation programs for many years prior to this pilot study. All subjects or guardians signed the informed consent approved by the University Institutional Review Board before participation.
Devices:
The study involved 2 types of BWSSs: a non-portable (BWSS1), and a semi-portable (BWSS2). Both BWSSs (Enliten LLC, Newark, DE) contained a custom harness that provided mechanical support and allowed the subjects to freely move throughout a 10ft x 10ft environment while preventing falls.
BWSS1: was setup at the child’s home, involved an overhead support rail system secured into the ceiling and a user-friendly counterweight system that allowed for the amount of body weight support to be adjusted by adding or subtracting weights on the base of the stack. The ceiling attachment and weight stack allowed the amount of support force to remain relatively constant as the child moved both horizontally and vertically. Thus the BWSS allowed for a range of mobility and physical activities throughout horizontal and vertical directions including: sitting, crawling, walking, jumping, and climbing.
BWSS2: was setup in the Go Baby Go café, a commercial business located within the atrium of the Health Science Complex building, at the University of Delaware (UD). The café, which serves beverages, ice cream, hot and cold snacks and soups, is a collaboration between the UD Creamery and our lab’s research program. As such, the café functions as both a business, research lab and rehabilitation environment to target physical, cognitive, social, language and/or vocational goals.
Study Design:
This pilot study involved case-series of the pediatric and adult subjects. Subjects used the BWSSs across multiple sessions over 2 months involving training on various tasks.
Pediatric case: The 2-month study involved a 3-week setup phase and a 7-week intervention phase, the latter being split in 2 sub-phases. The goals for the setup phase were to: i) ensure a safe environment for installation and modifications of the system, and ii) allow the child time to adjust and explore the new possibilities for play. The goal for the intervention phase was to promote lower limb weight-bearing and four-limb use through participation in physical activities and play with family.
The subject had daily access to the BWSS1 in the living room during both phases. The parents were asked to use the system to their convenience and the child’s tolerance. Feasibility and clinical outcome measures were assessed before, throughout and after completion of the study. Researchers visited the family’s home on a frequent basis to monitor the system’s effectiveness and perform assessments.
Adult cases: The 2-month intervention study involved 2-hour therapy sessions, 3 days per week in the Go Baby Go café. The overall goal was to engage subjects in various job activities that simultaneously required motor, social, communication and cognitive skills. Weekly goals were specifically aimed at improving upper and lower extremity functions, mental processing speed and/or communication. Thus, during each session, subjects greeted and served customers drinks and snacks, maintained food supplies at the counter and/or managed the register. Feasibility and clinical outcome measures were assessed before and at the end of each month of intervention.
Measures:
Feasibility was assessed from the caregiver and subject responses during interviews and activity logs, and investigators’ observations. Table 1 shows the different feasibility areas of focus (adapted from Bowen et al., 2009).
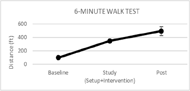
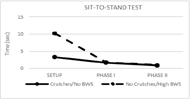
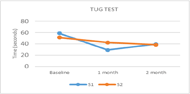
Clinical outcomes included the timed Sit-to-stand test (pediatric case only), the Timed Up and Go (TUG) test (adult cases only), and the 6-minute walk test (both populations). The Sit-to-Stand test is used to assess lower limb strength and balance (Wang, Liao & Peng, 2012). The TUG test is used to assess mobility, static and dynamic balance and to distinguish fallers from non-fallers (Shumway-Cook, Brauer & Woollacott, 2000). The 6-minute walk test is used to assess functional capacity and endurance (Solway, Brooks, Lacasse & Thomas, 2001).
| Areas of focus | Aims | Measures |
|---|---|---|
| Implementation | Were the BWSSs delivered as proposed? | Success/failure and time to setup the BWSSs |
| Practicality | Did the BWSSs provide a safe assistive environment as proposed? | Immediate effects on subjects’ movement and fulfillment of intervention goals |
| Acceptability | Were users and caregivers satisfied with their use of BWSSs? | Affect during use and estimated use of BWSSs |
| Demand | Did users and caregivers intent to continue use of BWSSs? | Intent to continue use of BWSSs |
| Adaptation | Could the BWSSs be applied across different environments and populations? | Time and features of BWSSs modified across different settings |
RESULTS
All subjects enjoyed participating in the study and were able to complete the 2-month intervention. All subjects had positive changes reported at all feasibility areas.
- Implementation: BWSS1 and BWSS2 were both setup within 2 weeks, and required relatively simple and minimal modifications to the wearable harness for comfort and performance.
- Practicality: Both BWSSs were successful in supporting subject movements for hours allowing them to focus on their goals throughout the study. No adverse events were reported and no repairs were required.
- Acceptability: In the pediatric case, the caregivers reported positive behavioral and emotional changes while engaging in physical activity in the BWSS1. The child was able to stand for 40 minutes to 1.5 hours per session.
- Demand: Caregivers and subjects expressed their willingness to either obtain a BWSSs at their home and/or continue volunteering at the Go Baby Go café after completion of study.
- Adaptation: Both BWSSs were successfully set up across different environments (home and work). In the pediatric case, the counterweight system proved to be useful as it provided body weight support so that the subject could move and interact. In the adult cases, a counterweight system was not required as the subjects preferred complete weight bearing.
Clinical Outcomes:
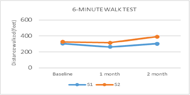
Adult population: Figure 3 shows no clear change in the 6-minute walk test throughout the study. Figure 4 shows a positive change in the TUG test with greater changes noted after 1 month of intervention. Subject 1 improved by 50% at 1 month to 33% at 2 months. Subject 2 improved by 23% at 1 month to 25% at 2 months.
DISCUSSION
Feasibility
Positive findings in the 5 primary areas of interest suggest the potential for feasible application of BWSSs in community spaces. For the pediatric case, using the BWSS1 was fun for the child and helped the child to be more interactive with his family. Family reported higher levels of function when the child used the BWSS compared to when he was outside the BWSS. For the adult cases, both subjects reported being satisfied with the BWSS2 because it prevented falls, allowed smooth movements and allowed them to focus on improving their physical, cognitive and communication abilities. Currently, both adult subjects continue to volunteer in the café twice a week.
Clinical measures
Pediatric case: The positive changes suggest that the new opportunities for physical activity and play experienced by the child while inside the BWSS1 created gains that may transfer to outside BWSS1 use.
Adult cases: Traditional approach to rehabilitation consists of giving various therapies at different hours of a day in an inpatient or outpatient clinical setting. The café with BWSS provided a novel approach where rehabilitation was integrated into work. The positive effect of working in this BWSS was seen through the different outcome measures used. For example, changes seen in the TUG test exceeded the MDC of >2.9 seconds for persons post-stroke (Flansbjer, Holmbäck, Downham, Patten, & Lexell, 2005). This suggests better dynamic balance and gait speed in both the subjects. However, we did not see any clear changes in the 6-minute walk test. Longer intervention and/or goals focused at increasing endurance may be needed for clear changes in some gait measures such as 6-minute walk test.
We advocate that incorporating real world harnesses in hospital, play, school and work settings would provide an immersive environment in which patients can develop both therapy goals AND life. One key research question is how community-based BWSSs compare in effectiveness with clinic-based BWSSs.
Study Limitations
Like any research study, there are limitations to the generalizability of our findings. First, the specific findings may not generalize to other contexts like home, school, work and recreational spaces. Second, findings of this study should not assumed to generalize to other neuro populations or even other subpopulations of TBI and Spina Bifida. Lastly, our short term findings may not generalize to more long term use. Future studies should consider the above limitations when developing specific research questions.
CONCLUSION
This report provides an initial foundation for a rehabilitation model with future research focusing on efficiency and effectiveness across various neurological sub populations. To our knowledge, this report is the first of its kind; a relatively intense, multi-domain rehabilitation approach used in a real world home and work setting to promote comprehensive recovery of different neurological population. Our study contributes to the development of intervention programs that merge the positive outcomes of body-weight supported training with the benefits of moving in enriched real-world environments. This technology application is scientifically significant, clinically established, and community driven. Future research will focus on testing more specific hypotheses and applying the BWSSs to other real world setting like playgrounds and recreational spaces.
REFERENCES
Cherng, R. J., Liu, C. F., Lau, T. W., & Hong, R. B. (2007). Effect of treadmill training with body weight support on gait and gross motor function in children with spastic cerebral palsy. American journal of physical medicine & rehabilitation, 86(7), 548-555.
Damiano, D. L., & DeJong, S. L. (2009). A systematic review of the effectiveness of treadmill training and body weight support in pediatric rehabilitation. Journal of neurologic physical therapy: JNPT, 33(1), 27.
Flansbjer, U. B., Holmbäck, A. M., Downham, D., Patten, C., & Lexell, J. (2005). Reliability of gait performance tests in men and women with hemiparesis after stroke. Journal of rehabilitation medicine, 37(2), 75-82.
Shames, J., Treger, I., Ring, H., & Giaquinto, S. (2007). Return to work following traumatic brain injury: trends and challenges. Disability and rehabilitation, 29(17), 1387-1395.
Shumway-Cook, A., Brauer, S., & Woollacott, M. (2000). Predicting the probability for falls in community-dwelling older adults using the Timed Up & Go Test. Physical therapy, 80(9), 896-903.
Solway, S., Brooks, D., Lacasse, Y., & Thomas, S. (2001). A qualitative systematic overview of the measurement properties of functional walk tests used in the cardiorespiratory domain. Chest Journal, 119(1), 256-270.
Wang, T. H., Liao, H. F., & Peng, Y. C. (2012). Reliability and validity of the five-repetition sit-to-stand test for children with cerebral palsy. Clinical rehabilitation, 26(a7), 664-671
Wrotniak, B. H., Epstein, L. H., Dorn, J. M., Jones, K. E., & Kondilis, V. A. (2006). The relationship between motor proficiency and physical activity in children. Pediatrics, 118(6), e1758-e1765.
ACKNOWLEDGEMENT
We thank the subjects and their families for their participation in this study, Steve Cope for developing the harness, Dr. Darcy Reisman for her valuable insight, undergraduate students for their assistance with data analysis, and Melinda Litvinas of UD creamery for collaborating with our lab for this research project. This work was partially supported by the UNIDEL 140 grant.