PRELIMINARY EVALUATION OF A MOBILE APP FOR EVERYDAY STROKE REHABILITATION
Sonia Lawson*, Jin Guo, Ted Smith, Ziying Tang, Jinjuan Feng
*Dept. of Occupational Therapy & Occupational Science,
Dept. of Computer and Information Sciences
Towson University
ABSTRACT
A smartphone-based rehabilitation approach called ARMStrokes was developed that provides real-time support for stroke survivors to complete rehabilitation exercises for upper extremity recovery. A pilot study of 10 stroke survivors was conducted to examine the usability and usefulness of the application. In addition, a web-based collaborative communication system was evaluated for usability and efficiency by therapists, physicians, and caregivers monitoring client adherence to prescribed home exercise programs. Post-test quantitative improvements were noted and feedback from focus groups involving stroke survivors, caregivers, and therapists have been positive. The findings assisted with modifications to the app and the collaborative system.
INTRODUCTION
Stroke is a major contributor to adult disability worldwide. According to the Centers for Disease Control and Prevention (CDC), more than 795,000 people in the United States have a stroke each year (2015). Stroke often causes long-term disabilities that affect cognitive, physical, and speech functions. A regular program of stretching and exercise is critical for stroke recovery during the early stage of a stroke. However, only 31 percent of stroke survivors actually complete the recommended exercises due to a variety of factors including lack of motivation (Shaughnessy, Resnick, & Macko, 2006). Interactive games such as the Nintendo Wii or 3D games can serve as a tool that is not only motivating but also used to meet therapeutic goals in a more engaging way (Kaminer, LeBras, McCall, Phan, Naud, Teodorescu, Kurniawan, 2014). Studies have shown that these types of game systems and haptic devices are effective in the rehabilitation process (Kam, Struzik, Jarus, & Rand, 2012). Access to these systems can be inconsistent and requires the individual to be in a specific location to be used for exercise. Physical capability to use the game systems may be limited due to poor postural control and standing balance resulting from the stroke, or cognitive impairment which limits understanding of the components to effectively play the games.
In contrast, smartphones can be easily carried to any place and do not require complicated installation or configuration processes. Although only 37 percent of people over 55 years old in developed countries owned a smartphone in 2013, the percentage is expected to exceed 80 percent by 2020 (Deloitt, 2014). Therefore, the smart phone can be used advantageously by stroke survivors to aid in their motor recovery. Individuals can play rehabilitation games delivered through mobile phones while watching TV, relaxing in the park, or even waiting for an appointment. In addition to the benefit of easy access, the mobile phone can also support timely communication between stroke survivors, therapists, and their caregivers, so that compliance to in-home exercise programs and progress can be monitored effectively from a remote location.
The smartphone-based rehabilitation approach called ARMStrokes was developed through close collaboration with stroke survivors and therapists. ARMStrokes is an interactive rehabilitation app that allows those with stroke to conduct rehabilitation exercises anytime and anywhere. It is designed to be used as a rehabilitation tool supervised by a licensed health care provider. Rather than using specialized sensors to track user movements, the focus was on developing an approach on top of existing mainstream technology without the need for any additional hardware. Movements are detected through the built-in sensors of common smartphones. ARMStrokes can also be easily customized to fit each stroke survivor’s specific functionality in different recovery stages. The following section describes the design of ARMStrokes.
APPLICATION DESIGN
ARMStrokes is implemented in the iPhone and Android environment; however, only the iPhone environment will be described in this paper The app uses built-in sensors of an iPhone (accelerometer, gyroscope, and device orientation sensor) to capture users’ movement speed and position information (e.g. pitch, roll and yaw value) during exercises.
Game Design
The app employs various methods to deliver feedback to users, including visual cues, audio cues, and haptic vibration. Stroke survivors can choose the type of feedback or feedback combinations that they prefer or that are prescribed by their therapists. They can also choose to disable the animation function to play the game with a static image on the screen.
Customized Rehabilitation
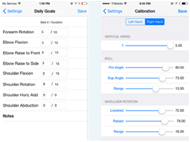
The goal of customized home exercises is achieved through two features: (1) a prescribed home exercise program (HEP) and (2) functional calibration. During a patient’s first visit, a therapist first conducts a thorough assessment of the patient’s functional capabilities such as muscle strength, active and passive range of motion in shoulder and elbow motions. The functional data allows the therapist to determine which app exercises are appropriate for the patient. Then the therapist develops a home exercise program for the patient that specifies the type of exercises, the number of sets for each exercise per day, and the length of each set. The HEP is entered into the app through the ‘Daily Goals’ page (Fig. 2). A specific daily goal not only provides a quantitative evaluation standard but also establishes observable achievement markers that motivate the users. Next, the functional data is used to set the appropriate calibration so that the movement of a patient with very limited range of motion or very slow speed can still be effectively detected (Fig. 2). Calibration information can also be used to detect intentional or unintentional cheating when the patient uses the unaffected arm to complete the exercises or performs movements incorrectly. Both the HEP and the calibration information need to be updated as the patient’s functionality gradually improves. This update can be performed by therapists from a remote location.
METHODOLOGY
Stroke survivors were recruited through multiple methods: stroke support groups, fieldwork contacts from an occupational therapy program, and dissemination of a video recording demonstration of the app. In addition, participants (i.e., occupational therapists, a physician, caregivers and stroke survivors) were recruited from a partnering inpatient rehabilitation center. Ten participants were included in the pilot study. These stroke survivors presented with stroke onset of within one year to up to 10 years. All participants received pre-testing of active and passive range of motion, muscle tone and strength, the Action Research Arm Test (ARAT), and the Chedoke Arm and Hand Inventory. The same measures were administered during a post-test at the end of the 6-week protocol in addition to a short interview to obtain qualitative data regarding the use of the app. Therapists and caregivers provided qualitative data at the end of the protocol.
All participants received training in use of the app and access to the website data. Researchers performed a 3-week check to ensure that participants were using the app and website properly, make adjustments as needed, and to answer any questions of the participants.
RESULTS AND DISCUSSION
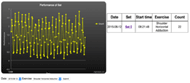
Other participants demonstrated similar improvements inactive range of motion and levels of fatigue at the end of the protocol. Improvement in functional ability as determined by the ARAT or Chedoke Arm and Hand Inventory were not significant at this point. Qualitatively, participants reported finding the app motivating as they could immediately see their performance level through observation of wave patterns that pop up at the end of each exercise along with repetition counts. Stroke survivors, caregivers, and therapists were able to easily access the web platform to monitor performance over a desired period of time.
Adapted straps were created to secure the phone to the affected arm if limited hand function was present. This proved to be the most challenging aspect for the technology. Because the phone needs to be held in a certain way for the motion to be detected by the phone, a strap with a wide variety of possible options to position the phone was essential. Several types were available from commercial sites for use by participants. Handmade straps were also fabricated.
Based on these pilot study results, the researchers plan to refine the way the phone can be secured to the affected limb, create automated calibration (eliminating the manual calibration process), and create new games and reminders that will help make the app more engaging. Plans also include expanding the application to other diagnostic groups and exploring the tele-rehabilitation implications. This research is ongoing and will advance to the use of an experimental design to truly determine the effectiveness of the app in improving upper limb recovery and function.
REFERENCES
Centers for Disease Control and Prevention. (2015) Stroke facts. Retrieved at: http://www.cdc.gov/stroke/facts.htm
Deloitt. The smartphone generation gap: over 55? There is no app for that. (2014) Retrieved at https://www2.deloitte.com/content/dam/Deloitte/global/Documents/Technology-Media-Telecommunications/gx-tmt-2014prediction-smartphone.pdf
Guo, J., Smith, T., Messing, D., Tang, Z., Lawson, S., and Feng, J. (2015) ARMStrokes: A mobile app for everyday stroke rehabilitation. Proceedings of ASSETS 2015. 429-430.
Kam, N., Struzik, J., Jarus, T., & Rand, D. (2012) Is the Nintendo Wii suitable for stroke rehabilitation? A pilot feasibility and usability study. The Israeli Journal of Occupational Therapy, 21(1), 3- 25.
Kaminer, C., LeBras, K., McCall, J., Phan, T., Naud, P., Teodorescu, M., Kurniawan, S. (2014) An immersive physical therapy game for stroke survivors. Proceedings of ASSETS 2014. 299-300.
Shaughnessy, M., Resnick, B.M., and Macko, R.F. (2006) Testing a model of post-stroke exercise behavior. Rehabilitation Nursing, 31(1), 15-21.
Tang, Z., Lawson, S., Messing, D., Guo, J., Smith, T., Feng, J. (2015) Collaborative rehabilitation support system: A comprehensive solution for everyday rehab. 2015 IEEE International Symposium on Multimedia. 61-64