Comprehensive, Technology- based, Team Approach for a Patient with Locked-In Syndrome: A Case Report of Improved Function & Quality of Life
Keara Savage, Madeline Lutjen, Kara Langhamer, Jeremiah Nieves, and Kimberly Hreha
Kessler Institute for Rehabilitation, West Orange, NJ
BACKGROUND
Stroke is one of the leading causes of disability in this country, with almost 800,000 people surviving each year (Mozaffarian et al., 2015). Thus, it is one of the largest groups treated in inpatient rehabilitation (Howlett, Lannin, Ada, & McKinstry, 2015; Nilsen, Gillen, Hreha, Osei, & Saleem, 2015). The most severe type of stroke seen in inpatient rehabilitation is locked- in syndrome (LIS) due to a loss of almost all functions and a high mortality rate (Casanova, Lazzari, Lotta, & Mazzucchi, 2003; Hoyer, Normann, Sorsdal, & Strand, 2010). The prevalence of LIS is unknown, but is estimated in the tens of thousands. LIS occurs typically from a brainstem lesion, specifically in the ventral pons after basilar artery occlusion, resulting in the preservation of consciousness and the complete loss of motor movement with the exception of vertical eye movements (Beaudoin & Serres, 2010). There are specific factors that have been correlated to better functional outcomes, for example: the recanalization of the basilar artery, early recovery of horizontal eye movement, and access to early multi-disciplinary rehabilitative treatment (Beaudoin & Serres, 2010; Leon- Carrion, van Eckhout, & Dominguez- Morales, 2002). However, there is still no known cure or standard treatment for people with LIS thus the prognosis is extremely varied.
| Discipline | Treatment/ Frequency | Description |
|---|---|---|
| PT | FES trial for the left lower extremity (LE) 1x/week | To strengthen the individual muscles (Doucet, 2012; Howlett et al., 2015). |
| OT/PT/ SLP | Increasing consistency of vertical eye gaze daily | For communication (Beaudoin & Serres, 2010). |
| OT/ SLP | Visual fixation/ horizontal visual tracking 4x/week | For communication (Beaudoin & Serres, 2010). |
| SLP | Basic oral motor movements/ volitional phonation daily | For communication (Beaudoin & Serres, 2010) |
| SLP | Thermal stimulation and ice chip trials daily | For improved swallowing (Leon- Carrion et al., 2002). |
Most of the research studies describe the following traditional therapy interventions for patients with LIS: preservation of range of motion/ limb mobilization, establishment of communication systems, and functional mobility training (Casanova et al., 2003; Schjolberg & Sunnerhagen, 2012).
Recently, technology has become a frequently- used adjunctive treatment for the general stroke population in inpatient rehabilitation and this technology is not limited to functional communication. For example: functional electric stimulation (FES), neuromuscular electrical stimulation (NMES), repetitive task practice, biofeedback, robotics, neuroprosthetics, robotic-assisted gait training (RAGT), and tablet technology (Doucet, 2012; Laffont, Bakhti, Coroian, van Dokkum, Mottet, Schweighofer, Froger, 2014; Nilsen et al., 2015).
PURPOSE
For the LIS population, there is no information regarding the use of the above technology for motor recovery other than for functional communication (Leon- Carrion et al., 2002; Schjolberg & Sunnerhagen, 2012). However, it may be applicable for people with LIS with evolving similar deficits to engage in these technologies. The purpose of this case report is to answer the following question: 1) Can the successful implication of an interdisciplinary, multi-sensory, multi-modal, technology based treatment approach to motor and communication deficits in a stroke survivor with LIS improve function and quality of life?
METHOD
This study was reviewed by an Institutional Review Board and deemed exempt. Research procedures included retrospective chart review. Demographic and clinical information was coded, de-identified and on a password-protected computer. Evaluation results, intervention, and outcome measures by the occupational, physical and speech therapists were summarized from the daily and weekly notes. The data was clustered at four time points, in order to facilitate visualization of his progression across a uniform time frame (Tables 1-3). The outcome measure used was the Functional Independence Measure (FIM), which measures the level of assistance the person requires. There are 18 items; the scores can range from 18 to 126 (independent). Each item is rated on a 7 point ordinal scale (Ottenbacher, Hsu, Grager, Fiedler, 1996). In addition, the patient’s family reported their interpretation of his quality of life on admission due to his inability to independently communicate. By discharge, report was completed by the patient.
| Discipline | Treatment/ Frequency | Description |
|---|---|---|
| OT | NMES to the right upper extremity (UE) 4x/week | For recovery of upper extremity function and increased functional outcomes (Doucet, 2012; Howlett, 2015). |
| PT | RTI FES cycling for bilateral lower extremities (BLE) 1-2x/week | To increase muscle strength, activate paretic muscles, reduce hypertonia, increase aerobic capacity, improve cardiopulmonary function, and improve symmetry (Ambrosini et al., 2012; Yeh, Tsai, Su, & Lo, 2010). |
| OT | RTI FES cycling for bilateral upper extremities (BUE) 1-2x/week | To promote the same effects as listed previously for lower extremities in the upper extremities of people recovering from hemiplegia after a stroke (Coupaud et al., 2008). |
| OT | Bioness H200 upper extremity neuroprosthesis for right hand and fingers 1-2x/week | To trigger a normal grasping pattern, improve functional arm use, reduce spasticity, and increase AROM in the effected upper extremity (Doucet, 2012) |
| OT | Cell phone access with switch control and micro- lite switch 3-4x/week | To increase independence in electronic aids to daily living and communication (Hreha & Snowdon, 2011). |
| OT | Repetitive task practice of self- feeding with the right UE 1-2x/week | To increase independence in ADLs (Nilsen et al., 2015). |
| OT/ PT | Trials in power wheelchair with head array 2-3x/week | To increase functional mobility (Schjolberg & Sunnerhagen, 2012). |
| SLP | NMES for swallowing structures 5x/week | To strengthen the striate musculature and improve swallowing function overall resulting in decreased reliance on gastrostomy feedings (Terre & Mearin, 2015). |
| SLP | Tablet technology training daily | To facilitate communication (White et al., 2015). |
| Discipline | Treatment/ Frequency | Description |
|---|---|---|
| OT | Armeo®Spring for left upper extremity motor control 1-2x/week | Repetitive task practice and visual feedback for improvements in self- monitoring, upper limb motor function, automatic motor responses, and sensory feedback patterns (Chang & Kim, 2013; Laffont et al, 2014; Nilsen et al., 2015). |
| PT | Lower extremity RTI FES cycling 2-3x/week | See Table 2 |
| PT | Gait training in the EksoTM 1x/week for 4 weeks | To improve lower limb function and functional ambulation, standing ability, motor FIM scores, walking distance, ADL performance, and overall gait function (Chang & Kim, 2013; Schwartz & Meiner, 2015). |
| PT | Lite Gait® training over ground with moderate bodyweight support 2x/ week | To increase postural control, gait function, cardiovascular fitness, ambulation distance, walking speed, and walking endurance (Hoyer et al., 2010; MacKay- Lyons, McDonald, Matheson, Eskes, Klus, 2013). |
| SLP | iPad access and use of voice output applications daily | For increased functional communication and to improve social communication (White et al., 2015). |
| SLP | Music therapy 3-4x/ week | To coordinate voice output leading to improvements in basic and social communication (Magee, 2014). |
Case
A.R. is a 39 year-old male, admitted to an inpatient rehabilitation facility with a primary diagnosis of LIS. The MRI imaging showed an occlusion of the vertebral artery as well as bibasilar. In the acute hospital, he had a successful mechanical thrombectomy. A.R. had no past medical history and was a healthy, active cyclist who worked full- time as an attorney.
RESULTS
Admission
On initial evaluation, A.R.’s total FIM score was a 17. He had low arousal and inconsistent eye opening on command. He was able to answer yes/no questions via vertical eye gaze inconsistently, when alert. He had no active movement in all four limbs, facial musculature, and cervical spine and presented with generalized hypotonicity. He presented with mild edema in bilateral lower extremities as well as clonus in left ankle. He was unable to swallow and required percutaneous endoscopy gastrostomy (PEG) for all nutrition, medication, and hydration.
Each day, A.R. participated in occupational, physical, and speech therapy for no less than 3 hours total time. This treatment was provided using a 1:1 model. The goals were set each week and reviewed by the team. A.R. played a part in goal setting. During the first 8 weeks, treatment targeted increased head control, visual tracking, and communication (Table 1). By the end of week 8, A.R. had a noticeable change in movement and was medically stable.
2 months
A.R. had increased head control and was able to complete neck active range of motion (AROM) in all planes independently. He had increased tone, including flexor tone in BUE and extensor tone in BLE. He had emerging right UE function in all joints. He could initiate right knee flexion/extension on command against gravity. A.R. tolerated upright on the tilt table at 80 degrees for up to 30 minutes. He was able to consume ice chips with supervision. He was able to initiate phonation to indicate yes/ no and nod/shake his head. A.R. had an overall FIM score of 26, with the most significant increases in cognitive domains. Due to the change in overall function, the treatment focused on motor retraining, including activity of daily living (ADL) task practice and functional mobility training (Table 2).
4 months
A.R. had significant gains in right UE strength, right LE strength, and trunk strength. He was able to access his cell phone, iPad, and letter board with use of the right UE independently, complete self- feeding with contact guard assistance, propel power wheelchair with right joystick, roll with moderate assistance, and complete squat- pivot transfers with moderate assistance. He had increased left shoulder strength. He was able to complete sit to stand in the parallel bars with minimal assistance. His diet was advanced to chopped solids and nectar thick liquids. He was able to produce phonetically loaded words/ phrases with fair to good intelligibility. A.R. had an overall FIM score of 59, with the most significant increases in functional mobility and upper body ADLs. At that point, treatment focused on increasing coordination on the right side and AROM on the left, as well as ADLs and functional mobility (Table 3).
Discharge
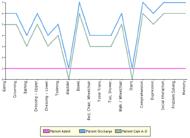
He was discharged to home with home care. His FIM motor score at discharge was a 54, indicating a gain of 42 points from admission. His total FIM score, including cognition, was 88, indicating a gain of 71 points from admission. In FIM cognitive scores alone, the patient gained 29 points (Figure 1).
DISCUSSION/CONCLUSION
Thirty years ago, the prognosis for LIS was poor, with almost 90% of patients dying within weeks of onset (Virgile, 1984). There are popular, commercialized accounts of people in a locked- in state such as the “Count of Monte Cristo” and “The Diving Bell and the Butterfly”, which elude the medical world to a one- sided view of LIS, with little hope for recovery (Cardwell, 2013).
According to the admission information regarding the patient in this case report, he was classified as having classic LIS. Besides having a successful thrombectomy and being in rehabilitation, A.R. was provided the opportunity to access both motor and communication sources, particularly through the use of various multi-modal technologies. This case report indicates that the combination of early use of these technologies, optimistic goal setting and treatments that were multi-modal, sensory and frequent, was essential to A.R.’s recovery. We understand the limitations to one specific case and thus recommend further research to make any specific recommendations or conclusions.
REFERENCES
Ambrosini, E., Ferrante, S., Ferrigno, G., Molteni, F., Pedrocchi, A. (2012) Cycling induced by electrical stimulation improves muscle activation and symmetry during pedaling in hemiparetic patients. IEEE Transactions On Neural Systems And Rehabilitation Engineering, 20(3), 320-330.
Beaudoin, N. & Serres, L. (2010). Locked-in Syndrome. International Encyclopedia of Rehabilitation. Retrieved from: http://cirrie.buffalo.edu/encyclopedia/en/article/303
Beninato, M., Gill-Body, K., et al. (2006). Determination of the minimal clinically important difference in the FIM instrument in patients with stroke. Archives of Physical Medicine and Rehabilitation, 87 (1): 32-29.
Cardwell, M. (2013). Locked-in Syndrome. The Journal of Texas Medicine, 109(2).
Casanova, E., Lazzari, R., Lotta, S., Mazzucchi, A. (2003) Locked-in syndrome: Improvement in the prognosis after an early intensive multidisciplinary rehabilitation. Archives of Physical Medical Rehabilitation, 84, 862-867.
Chang, W. H. & Kim, Y. (2013). Robot- assisted therapy in stroke rehabilitation. Journal of Stroke, 15(3), 174-181.
Coupaud, S., Gollee, H., Hunt, K., Fraser, M., Allan, D., &McLean, A. (2008). Arm- cranking exercises assisted by functional electrical stimulation in C6 tetraplegia: A pilot study. Technology and Health Care, 16, p. 415- 427.
Doucet, B. (2012). The issue is—Neurorehabilitation: Are we doing all that we can? American Journal of Occupational Therapy, 66, 488-493.
Hocker, S., Wijdicks, E. (2015). Recovery from locked- in syndrome. JAMA Neurology, 72(7), 832-833. dio:10.1001/jamaneurol.2015.0479.
Howlett, O., Lannin, N., Ada, L., McKinstry, C. (2015). Functional electrical stimulation improves activity after stroke: A systematic review with meta-analysis. Archives of Physical Medicine and Rehabilitation, 96, 934-943.
Hoyer, E., Normann, B., Sorsdal, R., Strand, L. (2010). Rehabilitation including treadmill therapy for patients with incomplete locked-in syndrome after stroke: A case series study of motor recovery. Brain Injury, 24(1), 34-35.
Hreha, K. and Snowdon, L. (2011) 'We All Can Call: Enhancing Accessible Cell Phone Usage for Clients with Spinal Cord Injury', Assistive Technology, 23: 2, 76 — 80.
Laffont, I., Bakhti, K., Coroian, F., van Dokkum, L., Mottet, D., Schweighofer, N., Froger, J. (2014). Innovative technologies applied to sensorimotor rehabilitation after stroke. Annals of Physical and Rehabilitation Medicine, 57, 543-551.
Leon-Carrion, J., van Eeckhout, P., Dominguez-Morales, M. (2002). The locked-in syndrome: a syndrome looking for a therapy. Brain Injury, 16, 555-569.
MacKay- Lyons, M., McDonald, A., Matheson, J., Eskes, G., Klus, M. A. (2013). Dual effects of Body Weight Supported Treadmill Training on cardiovascular fitness and walking ability early after stroke: A randomized controlled trial. Neurorehabilitation and Neural Repair, 27(7), 644-653.
Magee, W. (Ed.) (2014). Music technology in therapeutic and health settings. Philadelphia, PA: Jessica Kingsley Publishers.
Mozaffarian D, Benjamin E, Go A, et al. (2015). Heart disease, stroke and research statistics at- a- glance. Circulation.2015; 132.
Nilsen, D., Gillen, G., Hreha, K., Osei, E., Saleem, G.T. (2015) Effectiveness of interventions to improve occupational performance of people with motor impairments after stroke: An evidence- based review. American Journal of Occupational Therapy, 69(1), 6901180030.
Ottenbacher, KJ, Hsu, Y., Grager, C., Fiedler, R.C. (1996) The reliabiltiy of the functional independence measure: a quantitative review. Archives of Physical Medicine and Rehabilitatio, 77 (12): 127-32.
Schjolberg, A. & Sunnerhagen, K. (2012). Unlocking the locked in: A need for team approach in rehabilitation of survivors with locked in syndrome. Acta Neurologica Scandinavica, 125, 192-198.
Schwartz, I. & Meiner, Z. (2015). Robotic-assisted gait training in neurological patients: Who may benefit? Annals of Biomedical Engineering, 43(5), 1260-1269.
Terre, R. & Mearin, F. (2015). A randomized controlled study of neuromuscular electrical stimulation in oropharyngeal dysphagia secondary to acquired brain injury. European Journal of Neurology, 22, 687-696.
Virgile, R. (1984). Locked-in Syndrome: Case and literature review. Clinical Neurology and Neurosurgery, 86-4, 275-279.
White, J., Janssen, H., Jordan, L., Pollack, M. (2015). Tablet technology during stroke recovery: A survivor’s perspective. Disability and Rehabilitation, 37(13), 1186-1
Yen, C., Tsai, K., Su, F., Lo, H. (2010). Effect of a bout of leg cycling with electrical stimulation on reduction of hypertonia in patients with stroke. Archives of Physical Medicine and Rehabilitation, 91, 1731-1736.
ACKNOWLEDGEMENT
The authors would like to thank A.R. and his family for giving us permission to share his recovery.