Anh Dang, BS1; Evan Call, MS2
EC-Service1, Weber State University2Abstract
Aim: Pressure injuries frequently occur in hospital environments and can lead to secondary infections and complications in patient condition. The onset of pressure injuries is facilitated through the microclimate environment at the patient-surface interface of a full body support surface (i.e. a mattress, pad, and/or overlay). Specifically, the temperature and humidity are the primary contributors to microclimate conditions and, consequently, to the risk of pressure injury development. Standard testing methods aim to characterize microclimate conditions through the measurement of these two variables. Microclimate characterization is critical in the determination of a surface’s viability for use, especially with patients possessing a higher risk for pressure injury. Current methods employ the use of circulating water to delivery heat and moisture. A novel system is described to provide improved functionality without the sacrifice of repeatability and reliability—the Bronze Thermodynamic Rigid Loading Indenter (BTRLI).
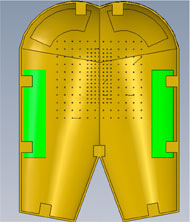
Materials: The BTRLI is casted from bronze to form the rigid buttock of the indenter. Microclimate conditions were assessed using four powered low air loss mattresses manufactured by KAP, Hill-Rom, and Freedom Medical.
Methods: Testing was performed in triplicate for three hours on each surface, with the BTRLI temperature maintained at 37 ± 1 °C and weighted to achieve a total load of 285 ± 10 N. The BTRLI was loaded with 200 mL of distilled water to provide consistent moisture delivery. Five sensors measured temperature and percent relative humidity (RH) were placed on the ischial tuberosities (ITs), perineum, and thighs of the indenter.
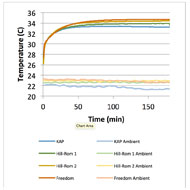
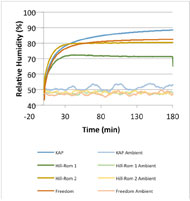
Results: Temperature and %RH measurements were similar for all support surfaces tested.
Conclusion: The BTRLI is a repeatable system, able to perform to specification during extended testing, providing reliable characterization for full body support surfaces.
Introduction
| Average Temperature (°C) | ||||
| 60 minutes | 120 minutes | 175 minutes | Max | |
| KAP | 33.3 ± 0.2 | 33.3 ± 0.2 | 33.2 ± 0.2 | 33.4 ± 0.3 |
| Hill-Rom 1 | 33.6 ± 0.1 | 33.8 ± 0 | 33.9 ± 0 | 33.9 ± 0 |
| Hill-Rom 2 | 34.1 ± 0.1 | 34.3 ± 0.1 | 34.4 ± 0.1 | 34.4 ± 0.1 |
| Freedom | 34.2 ± 0.1 | 34.6 ± 0.2 | 34.7 ± 0.1 | 34.7 ± 0.2 |
| Average Relative Humidity (%) | ||||
| 60 minutes | 120 minutes | 175 minutes | Max | |
| KAP | 83.1 ± 1.2 | 86.8 ± 0.6 | 88.3 ± 0.4 | 88.4 ± 0.4 |
| Hill-Rom 1 | 72 ± 0.7 | 71.3 ± 0.5 | 71.4 ± 0.3 | 72.4 ± 0.5 |
| Hill-Rom 2 | 80 ± 0.1 | 80.4 ± 0.1 | 80.4 ± 0.3 | 80.5 ± 0.2 |
| Freedom | 80.1 ± 0.5 | 81.9 ± 0.7 | 82.4 ± 0.8 | 82.5 ± 0.8 |
Clinical prevalence of pressure injury is a substantial issue in US healthcare. Pressure injuries account for approximately $6-15 billion in annual healthcare costs in the US (Markova & Mostow, 2012). In addition to monetary concerns, pressure injuries impose a great degree of discomfort and risk to patients, affecting up to 38, 23.9, and 17% of those in acute, long-term, and home care respectively (Jalali & Rezaie, 2005). Severely limited or restricted movement is a high pressure injury risk factor (Ferguson-Pell, Wilkie, Reswick, & Barbenel, 1980). Unrelieved pressure is one mechanism in the cascade of pressure ulcer development. Specifically, pressure injuries are a result of ischemic soft tissues evolving into open sores and skin lesions (Regan, Teasell, Wolfe, Keast, Mortenson, & Aubut, 2009). The breach in the dermis/epidermis and the chronic nature of pressure injury can frequently lead to secondary, and possibly life-threatening, infection (Russo, Steiner, & Spector, 2006).
Along with mechanical factors (such as pressure, friction, and shear), microclimate (temperature and moisture) conditions are implicated in pressure injury formation (Brienza & Geyer, 2005). Therefore, it is essential to characterize the microclimate of a full body support surface in order to assess its viability for patients with low-to-restricted mobility. The current US standard for microclimate testing of full body support surfaces is RESNA SS-1:2014 Section 3. It specifies the use of a Thermodynamic Rigid Cushion Loading Indenter (TRCLI) to load a support surface while delivering heat and moisture (ANSI/RESNA ). The indenter provides consistent microclimate delivery and a geometric shape analogous to the buttocks to simulate in vivo conditions (ISO/FDIS) (Ferguson-Pell, Hirose, Nicholson, & Call, 2009). However, using the TRCLI for multiple tests requires intensive maintenance. This manifests in the form of microbial growth or biofouling in the pores of the TRCLI moisture-permeable membrane—limiting function and eventually blocking moisture delivery completely. Another proposed indenter utilizes a plaster molded polyurethane indenter and a peristaltic pump to deliver moisture (Freeto, Cypress, Amalraj, Yusufishaq, & Bogie, 2016). An alternative system is described to alleviate the moisture delivery issue of the TRCLI and to provide a simple, but effective method for microclimate characterization—the Bronze Thermodynamic Rigid Loading Indenter (BTRLI).
Materials

Methods
Results
The BRLI performed to specification, allowing for the microclimate full body support surface characterization without failure or malfunction. Furthermore, the BTRLI maintained its reliability and demonstrated repeatability throughout the duration of the testing period. Figure 2 – Figure 4 and Table 1 illustrate the test data.
Discussion
No biofouling or microbial growth was observed while the BTRLI system was in use. Biofouling is one of the major and most cumbersome issues for the TRCLI. In the BTRLI, the moisture loaded evaporative towels provided a consistent method of moisture delivery, with little to no pore obstruction. In order to avoid microbial growth, the towels required drying after 8-12 hours of use. The BTRLI does face some limitations.
The most immediate limitation is the direct heating of the indenter perineum. The perineum is one of the warmest areas on the human body and the BTRLI system does not currently simulate that aspect. Another limitation is the corrosion of the bronze metal after repeated exposure to water. However, this is of little concern if maintenance is routine.
Conclusion
The BTRLI system is a repeatable and reliable alternative to the current TRCLI listed in microclimate testing standards. The system’s method of moisture delivery avoids the complications of membrane biofouling and integrated maintenance. Constant heat and moisture delivery is observed through the commercial full body support surfaces tested.References
ANSI/RESNA . (n.d.). Standard Protocol for Measuring Heat and Water Vapor Dissipation Characteristics of Full Body Support Surfaces - Body Analog Method. ANSI/RESNA SS-1:2014 .
Brienza, D. M., & Geyer, M. J. (2005, April). Using Support Surfaces to Manage Tissue Integrity. Advances in Skin and Wound Care , 151-157.
Ferguson-Pell, M., Hirose, H., Nicholson, G., & Call, E. (2009). Thermodynamic rigid cushion loading indentr: A buttock-shaped temperature and humidity measurement system for cushioning surfaces under anatomical compression conditions. Journal of Rehabilitation Research and Development , 46, 945-956.
Ferguson-Pell, M., Wilkie, I., Reswick, J., & Barbenel, J. (1980). Pressure Sore Prevention for the Wheelchair-Bound Spinal Injury Patient. Journal of Paraplega , 18, 42-50.
Freeto, T., Cypress, A., Amalraj, S., Yusufishaq, M., & Bogie, K. (2016). Development of a Sitting MicroEnvironment Simulator for wheelchair cushion assessment. Journal of Tissue Viability , 25, 175-179.
ISO/FDIS. (n.d.). Wheelchair seating - Part 2: Determination of physical and mechanical characterisitcs of devices intended to manage tissue integrity - Seat Cushions. ISO/FDIS 16840-2:2007 .
Jalali, R., & Rezaie, M. (2005). Predicting Pressure Ulcer Risk: Comparing the Predictive Validity of 4 Scales. Advances in Skin and Wound Care , 18, 92-97.
Markova, A., & Mostow, E. (2012). US skin disease assessment: ulcer and wound care. Dermatological Clinics , 30 (1), 107-111.
Regan, M., Teasell, R., Wolfe, D., Keast, D., Mortenson, W., & Aubut, J. (2009). A systematic review of therapeutic interventions for pressure ulcers after spinal cord injury. Archives of Physical Medicine and Rehabilitation , 90 (2), 213-231.
Russo, C. A., Steiner, C., & Spector, W. (2006). Hospitalizations Related to Pressure Ulcers among Adults 18 Years and Older, 2006. Healthcare Cost and Utilization Project. Agency for Healthcare Research and Quality.