The Impact Of Small Changes In Seating Posture On Skin Vitality
Iris Hoogendoorn1,2, Jasper Reenalda2, Bart F.J.M. Koopman1, Jaap H. Buurke1,2, Hans S. Rietman1
1 University of Twente, Enschede, the Netherlands
2 Roessingh Research & Development, Enschede, the NetherlandsBackground
Prolonged sitting, and a sedentary lifestyle in general, has detrimental effect on the human body, it increases the risk for diabetes, cardiovascular and chronic diseases, frailty, morbidity and mortality (Hamilton, Healy, Dunstan, Zderic, & Owen, 2008; Owen, Healy, Matthews, & Dunstan, 2010; Van Uffelen et al., 2010; Wilmot et al., 2012). And for those with limited mobility or sensory function, prolonged sitting induces a high risk of tissue damage and could eventually lead to pressure ulcer development (Coleman et al., 2013; NPUAP & EPUAP, 2009).
While seated, the pressure under the seat and especially around the bony prominences of the ischias tuberositas increases, resulting in compression of the tissue and blockage of the microcirculation. To prevent tissue damage it is essential to reduce the (peak) pressure under the seat and offload the tissue in time (Whittemore, 1998). Healthy young individuals reduce the sitting load by moving or re-sitting every 8 minutes, on average (J Reenalda et al., 2009). And for those with limited mobility or sensory function there are pressure reducing cushions to reduce and redistribute the pressure under the seat. But for those that cannot move or reposition in time independently, a pressure reducing cushion is probably not enough to offload the tissue and prevent tissue damage. These persons will need a more dynamic system that actively changes the load distribution under the seat. An example of such a system is the experimental ‘Dynasit chair’, that independently controls the seating posture to redistribute the load and increase perfusion under the tubera (Jasper Reenalda, van Geffen, Snoek, Jannink, & Rietman, 2010; van Geffen, Reenalda, Veltink, & Koopman, 2008). But this chair was built for experimental purpose and is in its current form not suitable for clinical practice. Another option for offloading is a backwards tilt or recline of a chair. Previous studies show that tilting angles of 30° or more backwards are beneficial for increasing tissue viability and relieve the pressure under the tubera (Henderson, Price, Brandstater, & Mandac, 1994; Jan, Jones, Rabadi, Foreman, & Thiessen, 2010; Sonenblum & Sprigle, 2011). But these large postural changes can be very disturbing for the user, as they could interfere with daily and social activities.
Therefore is the objective of this study whether small changes in seating posture also can increase tissue viability and counteract the effects of long term sitting in healthy young subjects. A normal motorized care-chair with stand-up module is the starting point of this study to assure feasibility in practice.
Methods
Subjects
Ten healthy young (age 26±4 years, weight 71±9 kg, length 1.78±0.9 m, 5 male, 5 female) subjects were recruited for this study from the local university. Criteria for exclusion were smoking, skin conditions, vascular disease (e.g. diabetes) or an operation on the lower back or seat. Prior to the experiment, all subjects read and signed an ‘informed consent’ in which the objective and experimental protocol was explained. The protocol was approved by the Medical and Ethical Committee of MST Enschede, the Netherlands.
Experimental set-up
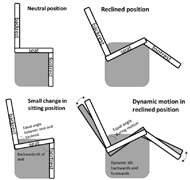
To investigate the effect of automatically imposed changes in seating posture on the skin viability under the tubera, an electrical-controlled care-chair (Vario fitform, WELLCO international BV, the Netherlands) was connected with an operating system (Wi-Fi connection to a laptop or tablet) controlling the motions of the chair. The operating system allowed for control of the back rest and seat angle, folding and unfolding of the footrest and actuation of the stand-up module. The measurement conditions were preprogrammed in the operating system and when actuated by the researcher the chair automatically changed the seating position, and thereby the seating posture of the subject.
Tissue viability was measured with two sensors connected to the Oxygen to See (O2C, LEA medizintechnik Giessen, Germany). The O2C combines Laser Doppler Flowmetry (830nm and 30mW) and White light tissue spectroscopy (500-800nm; 1nm resolution; 20W) for non-invasive measurement of tissue oxygenation and skin blood flow. The two sensors allow simultaneous measurement at two measurement depths; approximately 1 mm depth (superficial or cutaneous) and maximal 8 mm depth (deep or subcutaneous). Each sensors was placed at the skin under the ischias tuberositas (superficial sensor on the left, deep sensor on the right).
Protocol
Data analysis
The tissue viability data of the O2C is analyzed in MatLab 2014b. Missing values were estimated using linear interpolation and the baseline during normal sitting was calculated. All experimental conditions are normalized by this baseline. For each condition are the mean oxygenation and blood flow (superficial and deep) calculated per subject. Hereafter total group means were calculated per condition. Statistical testing was done in IBM SPSS statistics version 22 with α=5%. To test whether the static and dynamic conditions were statistical different from normal sitting a one-sample T-test is performed. To test for statistical difference between the tilting angles a repeated measurement analysis was performed.
Results
During the baseline measurement in neutral position, the oxygenation was superficially 46.7±16.5% and deep 62.5±11.0% and the blood flow was superficially 23.8±15.3 AU and deep 90.9±41.1 AU for the total group of 10 healthy young subjects. All other conditions are normalized to the baseline values of sitting in neutral position.
Part 1: small changes in sitting position
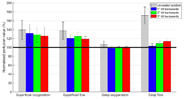
The three tilt angles are only significant different from neutral position for superficial blood flow (1° t(9)=2.308 p=0.046; 2° t(9)=2.616 p=0.028; 3° t(9)=2.962 p=0.016). And no significant difference was shown between the three tilt angles.
Part 2: dynamic motion in reclined position
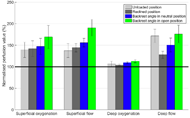
Table 1. Statistical results of part 2 dynamic motions in reclined position compared to sitting in neutral position.
Discussion
|
|
Difference with neutral position | ||
|---|---|---|---|---|
| (µ) | t (9) | p-value | ||
| Superficial oxygenation | normal | 42.0 | 1.964 | 0.081 |
| open | 47.3 | 2.004 | 0.076 | |
| Superficial blood flow | normal | 56.2 | 4.395 | 0.002* |
| open | 90.6 | 3.671 | 0.005* | |
| Deep oxygenation | normal | 9.4 | 3.278 | 0.010* |
| open | 12.9 | 2.628 | 0.027* | |
| Deep blood flow | normal | 50.5 | 2.434 | 0.038* |
| open | 76.1 | 2.887 | 0.018* | |
The goal of this study was to investigate whether small changes in seating position have a positive effect on skin vitality. Previous studies have shown that tilting angles of 30° or more increase skin perfusion and adequately change the location of peak pressure (Henderson et al., 1994; Jan et al., 2010; Sonenblum & Sprigle, 2011). But these motions do interfere with daily and social activities and are therefore not feasibly in daily live. In this study the changes in seating posture were very small (total range from 2° to 6° tilt backwards) allowing the person to continue daily activities as the trunk and head remained in an upright position. Overall we can conclude that these small changes in seating position increase tissue viability in healthy and young subjects. Most increase was seen in the superficial oxygenation and superficial blood flow and to a much lesser degree in the deeper measurements (max 8 mm depth). Furthermore, we expected that larger tilt angles would results in a more positive effect on skin vitality, but this was not indicated. This could be related to the shape of the tubera (Linder-Ganz et al., 2008); with the tilt the peak pressure under the tubera shifts backwards and depend on the curvature and shape of the tuber a larger or smaller tilt could be more beneficial.
The addition of a dynamic motion (a rocking motion) to the static reclined position resulted in a large increase in skin vitality (superficially and deeper in the tissue). Increasing the recline angle (the angle between backrest and seat) shows a clear effect on skin vitality. The increase in tissue viability due to recline could be two-fold. Firstly, it leads to a larger hip angle, allowing easier blood flow through the larger arteries deep in the pelvis. Secondly, a larger recline change the relative location to the heart, allowing for better circulation. But the downside of recline could be an increase in load shear stress due to movement between trunk and lower extremities (Aissaoui, Lacoste, & Dansereau, 2001; Goossens, Snijders, Holscher, Heerens, & Holman, 1997; Hobson, 1992).
Future work will comprise extension of this research to an elderly population as age is considered as a risk factor for tissue injury due to an increase in skin stiffness and changes in cardiovascular capacity and microcirculation (Daly & Odland, 1979).
Conclusion
We can carefully conclude from this study that small tilts backwards have a positive effect on tissue viability. But as the tissue is not completely off-loaded, the timing for these changes in posture will be crucial. We expect that the small tilts should be performed more often than the current guideline for changing position. Keeping in mind the sitting behavior of healthy subjects, who on average change position every 8 minutes, could be of guidance.References
Aissaoui, R., Lacoste, M., & Dansereau, J. (2001). Analysis of sliding and pressure distribution during a repositioning of persons in a simulator chair. IEEE Transactions on Neural Systems and Rehabilitation Engineering, 9(2), 215–224.
Coleman, S., Gorecki, C., Nelson, E. A., Closs, S. J., Defloor, T., Halfens, R., … Nixon, J. (2013). Patient risk factors for pressure ulcer development: Systematic review. International Journal of Nursing Studies, 50(7), 974–1003.
Daly, C. H., & Odland, G. F. (1979). Age-related Changes in the Mechanical Properties of Human Skin. Journal of Investigative Dermatology, 73(1), 84–87.
Goossens, R. H. M., Snijders, C. J., Holscher, T. G., Heerens, W. C. W., & Holman, A. E. (1997). Shear stress measured on beds and wheelchairs. Scandinavian Journal of Rehabilitation Medicine, 29(3), 131–136.
Hamilton, M. T., Healy, G. N., Dunstan, D. W., Zderic, T. W., & Owen, N. (2008). Too Little Exercise and Too Much Sitting: Inactivity Physiology and the Need for New Recommendations on Sedentary Behavior. Current Cardiovascular Risk Reports, 2(4), 292–298.
Henderson, J. L., Price, S. H., Brandstater, M. E., & Mandac, B. R. (1994). Efficacy of three measures to relieve pressure in seated persons with spinal cord injury. Archives of Physical Medicine and Rehabilitation, 75(5), 535–9.
Hobson, D. a. (1992). Comparative effects of posture on pressure and shear at the body-seat interface. The Journal of Rehabilitation Research and Development, 29(4), 21.
Jan, Y.-K., Jones, M., Rabadi, M., Foreman, R., & Thiessen, A. (2010). Effect of Wheelchair Tilt-in-Space and Recline Angles on Skin Perfusion Over the Ischial Tuberosity in People With Spinal Cord Injury. Archives of Physical Medicine & Rehabilitation, 91(11), 1758–1764.
Linder-Ganz, E., Shabshin, N., Itzchak, Y., Yizhar, Z., Siev-Ner, I., & Gefen, A. (2008). Strains and stresses in sub-dermal tissues of the buttocks are greater in paraplegics than in healthy during sitting. Journal of Biomechanics, 41(3), 567–80.
NPUAP, & EPUAP. (2009). European Pressure Ulcer Advisory Panel and National Pressure Ulcer Advisory Panel. Prevention and treatment of pressure ulcers: quick reference guide. Washington DC: National Pressure Ulcer Advisory Panel.
Owen, N., Healy, G. N., Matthews, C. E., & Dunstan, D. W. (2010). Too much sitting: the population health science of sedentary behavior. Exercise and Sport Sciences Reviews, 38(3), 105–13.
Reenalda, J., Geffen, P., Nederhand, M., Jannink, M., Ijzerman, M., & Rietman, H. (2009). Analysis of healthy sitting behavior: interface pressure distribution and subcutaneous tissue oxygenation. Journal of Rehabilitation Research & Development, 46(5), 577–586.
Reenalda, J., van Geffen, P., Snoek, G., Jannink, M., & Rietman, H. (2010). Effects of dynamic sitting interventions on tissue oxygentation in individuals with spinal cord disorders. Spinal Cord, 48(4), 336–341.
Sonenblum, S. E., & Sprigle, S. H. (2011). The impact of tilting on blood flow and localized tissue loading. Journal of Tissue Viability, 20(1), 3–13.
van Geffen, P., Reenalda, J., Veltink, P. H., & Koopman, B. F. J. M. (2008). Effects of sagittal postural adjustments on seat reaction load. Journal of Biomechanics, 41(10), 2237–2245.
Van Uffelen, J. G. Z., Wong, J., Chau, J. Y., Van Der Ploeg, H. P., Riphagen, I., Gilson, N. D., … Brown, W. J. (2010). Occupational sitting and health risks: A systematic review. American Journal of Preventive Medicine, 39(4), 379–388.
Whittemore, R. (1998). Pressure-reduction support surfaces: a review of the literature. Journal of Wound, Ostomy & Continence Nursing, 25(1), 6–25.
Wilmot, E. G., Edwardson, C. L., Achana, F. A., Davies, M. J., Gorely, T., Gray, L. J., … Biddle, S. J. H. (2012). Sedentary time in adults and the association with diabetes, cardiovascular disease and death: Systematic review and meta-analysis. Diabetologia, 55(11), 2895–2905.
Acknowledgement
This research is supported by the Dutch Technology Foundation STW, which is part of the Netherlands Organization for Scientific Research (NWO), and which is partly funded by the Ministry of Economic Affairs (12673) and by the REAP (Regionaal Economisch Actie Programma) from the MRE (Metropool Regio Eindhoven).
Conflict of Intereset
There are no commercial relationships which may lead to a conflict of interest with any of the authors.