MOBILE ASSISTANT FOR ALZHEIMER PATIENTS
ABSTRACT
The use of pervasive computing elements such as java smart phones and multi-modal sensors in smart homes of the future can potentially assist patients with Alzheimer's Disease (AD). We present an ongoing research project whose goal is to create a cognitive assistant to improve the independence of live-at-home AD patients. The architecture of the Mobile Patient Care-Giving Assistant (mPCA) integrates local-positioning systems, J2ME-based smart phones and wireless and visual sensors.
BACKGROUND
Alzheimer disease is a dementing disorder, characterized by cognitive and behavioral decline. It involves the damage, breakdown of connections, and death of brain cells, impacting memory, thought, and language. Other symptoms include difficulty with abstract thinking, disorientation, loss of judgment, and personality changes. People with moderate AD may have great difficulty functioning without supervision. One in ten elders in the US suffer from AD. It is estimated that 1 in 5 elders will have AD by 2050. In 2002 AD will have resulted in health related expenditures of more than $61B [1].
At the University of Florida (UF) RERC on Technology for Successful Aging we are exploring the use of pervasive and wireless technology to create a mobile patient care-giver assistant (mPCA). Our goal is to create a tool to reduce caregiver burden. The mPCA assistant is a smart phone that interacts with a set of sensors in a smart space, in which most of the computation, decisions, and events take place. The mPCA will assist persons with AD in daily activities by means of reminders, orientation, and context-sensitive teaching, and monitoring.
APPROACH
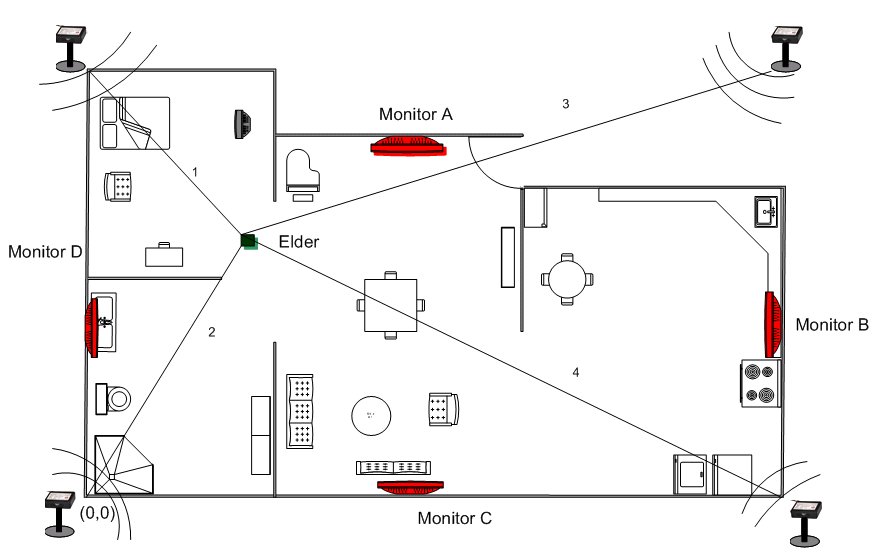
In-door Tracking system. mPCA is based on an ultrasonic indoor tracking system, already implemented in an elder house model at UF. It operates in the ultrasonic range (40 KHz). The system, shown in Figure 1, consists of: (1) four fixed devices (known as pilots or monitors) located in each corner of each room in the house, and (2) two moving devices (known as tags or beacons), which are placed on the shoulders of a light-weight "net" vest worn by the elder. The four pilots acts as receivers that receive signals from the beacons. The position of the beacons is calculated based on the two shortest times that the ultrasonic waves take from the beacon to the pilots and a trilateration technique (see line labeled 1 and 2 in Figure 1). By using two beacons, the system not only is able to detect the position of the elder, but also his/her orientation. Other related technologies include smart phones and other sensors.
 |
The mPCA system is designed as a smart phone with static IP address and a speakerphone. It is also assumed that the battery of the smart phone can last for a full day. This is not currently possible without using additional standard batteries. The mPCA assists AD patients by performing the following four functions, as needed or as requested:
As a reminder for critical tasks (to take medications, to eat at meal times, to visit a doctor, to call son on his birthday, to feed pet, etc). This function is proactive, thus does not require patient initiation.
As a teaching tool to perform step-by-step tasks. For instance, provide instructions for using a microwave oven to cook a meal, or perform hygienic routines or operate a VCR. This function is also proactive but requires context information. For instance, time and location information can trigger the step-by-step hygiene procedure reminders. Context information is supplied by the smart house.
As a location tracking mechanism to locate the patient in the house as well as important objects such as medications. Some of this functionality is passive, while some may require the patient request.
As a monitoring tool to record the activities performed by the elder. Here mPCA acts proactively but does not interact with the elder.
COMPONENTS OF mPCA
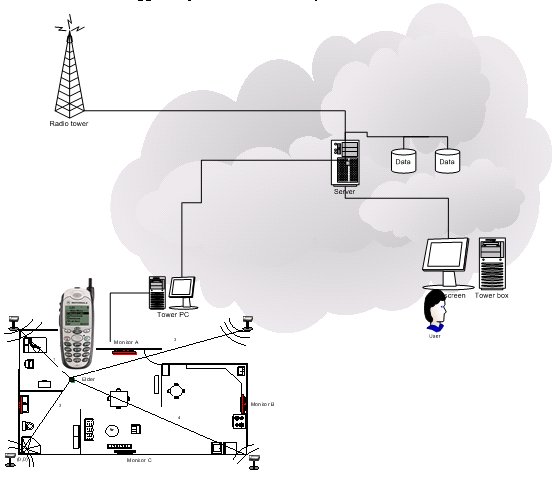
Figure 2 shows the different components of the mPCA system. A computer (server) is connected to local sensors such as monitors, speakers and an ultrasonic location tracking system. The home server is also connected to the Internet through a broadband technology. A smart phone with routable IP is also connected to the smart house through a wireless data service plan. The smart phone coordinates with the home server to detect contexts, respond to AD patient's request, or to capture attention and deliver a message to the patient. Additionally, a remote monitoring facility can be attached to mPCA to store history information on patient activities. Patient interaction with mPCA can also be logged to provide data to study the effectiveness of the mPCA tool.
 |
-
Koppel R. Alzheimer Disease: The cost to U.S. Businesses in 2002. Alzheimer's Association.2002.
-
Hopper, T.; Bayles K.; Kim E. Retained Neuropsychological Abilities of Individuals with Alzheimer's Disease. Seminars in Speech and Language 22(4): 261-270, 2001
ACKNOWLEDGEMENTS
This research was supported through funding from the National Institute on Disability and Rehabilitation Research of the U.S. Department of Education and the Administration on Aging of the Department of Health and Human Services.
Giraldo,
Carlos
Computer & Information Science & Eng. Department
University of Florida, Gainesville,
FL 32611
(352) 392-6845, Fax: (352) 392-3238
helal@cise.ufl.edu
