Inertial Motion Sensors as Building Blocks for Wearable Assist Devices
ABSTRACT
The miniaturization of electronics has allowed the creation of new biofeedback assist devices that can be worn on a belt and even embedded into clothing without affecting the wearer's ability to perform normal daily activities. To detect and predict balance instabilities in individuals with acquired brain injury, algorithms are being developed to track and interpret human movement using a miniature commercial motion sensor that provides real-time 3D orientation data. This paper validates the usefulness of an inertial motion sensor for detecting complex three dimensional motion in a portable manner. The ultimate goal is to include these sensors into a portable, wearable assist device that will be used for therapy, research, and treatment of individuals with brain injury.
KEYWORDS:
balance, motion sensors, assist device
BACKGROUND/PURPOSE
Balance instabilities can occur for a variety of reasons. Deficits of the visual, proprioceptive, vestibular, or motor control systems can significantly impair an individual's ability to sit, stand or walk without losing balance. Biofeedback has been shown to improve balance control in some populations; however, its applicability is limited because current rehabilitation devices are not portable. Existing devices for therapy provide balance biofeedback using forceplates coupled with visual, tactile, or auditory feedback to the user. However, no commercially-available portable balance assist device exists. A portable device would be significant because it can be used to practice balance control outside of physical therapy sessions. Prototype wearable balance feedback devices have been reported using a head-mounted accelerometer and gyroscope to measure changes in head tilt, or with biofeedback via tactile actuators on the shoulders or trunk in healthy subjects (1). The use of haptic feedback on the tongue has been used to compensate for vestibular damage (2). Creating generalized biofeedback algorithms for use in the brain injury population is likely to be challenging because a wide array of physical and cognitive disorders can accompany brain injury.
The first step in creating an assist device is to identify appropriate sensors, then to develop the biofeedback methods and hardware, and finally, to integrate the elements into a lightweight, portable unit. Accelerometers have been used for many years to detect movements and changes in balance of the human body (3,4). The inclusion of accelerometers into consumer products and automobiles has made them a low-cost option for commercial rehabilitation assist devices. However, accelerometer-based measurement systems are affected by sensor variability, systematic errors, noise, and the effect of gravity (5). Determining absolute position is difficult because integration of the acceleration signals introduces cumulative position error (6). To compensate, gyroscopes may be used singly or in conjunction with accelerometers to compensate for gravity effects and to measure changes in body position and trunk angle (7).
APPROACH
 |
|---|
The MT9 Real-time 3D Motion Tracker was selected to avoid limitations with accelerometers; it is a compact miniature inertial sensor that was designed to track human motion. The MT9 sensor measures rate-of-turn (using gyroscopes), acceleration (using accelerometers), and Earth magnetic field (using magnetometers) and eliminates position drift to provide accurate, calibrated orientation data in real time. Working with the sensor is straightforward; calibrated data can be integrated into custom software using an optional software developer's kit, or can be imported into existing applications such as Microsoft Excel.
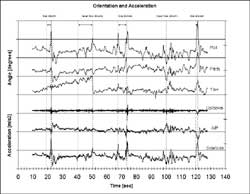
Data has been collected from a healthy individual with no balance instabilities. The sensor was secured on the torso below the collar bones. For illustration, the approximate position is shown in Figure 1. The subject was asked to stand on one foot with eyes closed. Although this is a somewhat artificial situation, it is one of several scenarios being used to develop the instability detection algorithm, and is used for illustration. In Figure 2, three axes of acceleration data are shown on the bottom, and three axes of orientation data on the top (roll, pitch, and yaw). As expected, side-to-side motion is the largest, with moderate anterior/posterior (A/P) movement. At three times during the 120 second trial, the subject lost balance and had to momentarily place her other foot on the ground to regain balance (toe-down). Near loss-of-balance occurred two times. These five events are noted in the figure with solid dashed lines.
OUTCOME/PERFORMANCE & COST
 |
|---|
Several conclusions can be drawn regarding how these signals should be interpreted. Since loss-of-balance and near loss-of-balance are characterized (in this scenario) by side-to-side accelerations larger than +/- 2 m/s ², a simple algorithm could simply scan for acceleration values that exceed a predefined threshold in one or more axes (directions). However, we find that accelerations exceed this value during normal activities like moving objects around on a table. Also, by the time a large acceleration is detected using a threshold, it is often too late to provide a warning to the subject.
Care must also be taken when attempting to interpret the orientation signals. The orientation values that are calculated every 10 milliseconds are only instantaneous measures of orientation of the sensor, and not a measure of angle offset from the vertical standing position. It may be tempting to set a threshold on pitch angle, for example, and classify all angles greater than 10 degrees as potential fall conditions. However, it is possible to lean backwards at this pitch (triggering a false warning) and still maintain the position of the sensor (and the center of mass of the subject) well within the base of support in a controlled manner.
The initial results of the basic instability algorithm show it is able to detect all three of the toe-down events before they occurred, and one of the two near loss-of-balance events. Early warnings predicted by the algorithm are shown as lighter dotted lines in Figure 2. Of the three toe-downs, only two were likely detected in enough time to provide feedback (1.7 sec and 3.2 sec), while the last (at less than 1 second) would have failed. One near toe-down was detected 10 seconds before a toe-down occurred, while the other was not detected at all. We are developing a more robust method that considers temporal features such as change in orientation, symmetry in multiple signals, and oscillatory instabilities in order to classify movement types and to provide early warning of instabilities without false detections.
At this time, it is technologically possible to develop a lightweight portable assist device using this sensor, although the cost of the entire device will still exceed $4,000 if commercially produced in small volumes. In its current configuration, the sensor requires a 5.5V supply voltage and draws 40 milliamps. To make a portable system, the sensor must connect to a small single board computer that will process and interpret data in real time, make posture/balance recommendations, and then provide biofeedback to the user via some hardware output device (e.g., using visual or tactile feedback). Using the latest low power devices and battery technology, batteries will still need to be replaced daily for full-time usage. However, steady advances in miniaturization and battery technology will make this device an affordable reality in the near future.
IMPLICATIONS/FUTURE DIRECTIONS
We intend to continue research and development using this sensor configuration during different user scenarios and with individuals having injury-related balance instabilities. Ultimately, the device will be integrated into a wearable biofeedback system to track balance instabilities in real time, and to provide feedback to the wearer when balance or mobility appears to be compromised. In addition to this commercial goal, the device is part of a hardware/software platform for rehabilitation research in mobility disorders for individuals with brain injury.
REFERENCES
- Wall III, C., Weinberg, M.S., Schmidt, P.B., & Krebs, D.E. (2001). Balance prosthesis based on micromechanical sensors using vibrotactile feedback of tilt. IEEE Transactions on Biomedical Engineering, 48(10), 1153-61.
- Bach-y-Rita, P. (1998). Form perception with a 49-point electrotactile stimulus array on the tongue: A technical note. Journal of Rehabilitation Research and Development, 35(4), 427-430.
- Cho, C.-Y. & Kamen, G. (1998). Detecting balance deficits in frequent fallers using clinical and quantitative evaluation tools. Journal of the American Geriatrics Society, 46(4), 426-430.
- Veltink, P.H., Bussmann, B.J., de Vries, W., Martens, W.L.J., & Van Lummel, R.C. (1996). Detection of Static and Dynamic Activities Using Uniaxial Accelerometers. IEEE Transactions on Rehabilitation Engineering, 4(4), 375-385.
- Moe-Nilssen, R. & Helbostad, J.L. (2002). Trunk accelerometry as a measure of balance control during quiet standing. Gait and Posture, 16(1), 60-68.
- Giansanti, D., Macellari, V., Maccioni, G., Cappozzo, A. (2003). Is it Feasible to Reconstruct Body Segment 3-D Position and Orientation Using Accelerometric Data? IEEE Transactions in Biomedical Engineering, 50(4), 476-483.
- Najafi, B., Aminian, K., Loew, F., Blanc, Y., & Robert, P.A. (2002). Measurement of stand-sit and sit-stand transitions using a miniature gyroscope and its application in fall risk evaluation in the elderly. IEEE Transactions in Biomedical Engineering, 49(8), 843-851.
Author Contact Information:
Lisa K. Simone, Ph.D.,
Kessler Medical Rehabilitation Research and Education
Corporation,
1199 Pleasant Valley Way,
West Orange, NJ 07052,
Office Phone (973) 324-3550,
EMAIL: lsimone@kmrrec.org
