Technologically Delivered Cognitive Assistance with Activities of Daily Living
ABSTRACT
Previous studies have explored the benefits of cueing persons with cognitive impairment including use of computerized cues. The purpose of this project was to study the use of machine-based cues to persons with moderate cognitive impairment to complete self-care tasks of varying complexity. Persons with moderate cognitive impairment responded positively to machine-based cues. Some participants required more than one cue for safety. Machine-based cueing has promise for increasing the level of independence for people with dementia.
KEY WORDS
Cognitive impairment, self-care tasks, cuing, care-giver burden, technologically delivered cues
BACKROUND
Approximately 10% of people over the age of 65 have cognitive impairments that impact on their functional abilities. Dementia is a broad term to describe a decline in intellectual functioning that is not a normal part of the aging process. , Alzheimer's disease is the most common cause of dementia in persons over 65, and strokes are the second most frequently occurring type of dementia.
As Alzheimer's disease progresses it impacts on a person's independent function. A person with Alzheimer's disease will decline in ability to meet safety, self-care, household, leisure, social interaction and vocational needs. Eventually, the person will lose the ability to perform basic activities of daily living. Dementia impacts not only on persons with cognitive impairment but also on their family members. Poor health of family members, and lack of knowledge or information of the disease process also impact on caregiving burden.
For most persons with Alzheimer's disease, the home is the major setting where care is provided and family members are their primary care providers. Research documents the need for support for caregivers of persons with cognitive impairments. Tasks performed by family members for persons with cognitive impairment range from self-care activities (bathing, dressing), instrumental daily living activities (money management, meal preparation) to decision making.
An emerging area of research is focused on assisting persons with cognitive impairments in their daily activities through the use of computerized devices. Mihailidis et al. developed a computerized cueing device to assist with the task of hand washing in elderly persons with dementia. The computerized system consisted of a nine step verbal prompting device equipped with transducers to monitor step completion, and did not require user input or intervention for effective operation. Another study reported that patients improved in independence in dressing, and increased participation in dressing when prompted. Engleman et al. found increasing opportunities for independent activity with severely cognitively impaired elders, using more nondirective and directive verbal assists rather than physical assists, independence was increased. These studies suggest that persons with cognitive impairment benefit from cueing in task performance and that computerized cuing is possible.
RESEARCH QUESTION
The purpose of this project was to determine appropriate users with cognitive impairment for a smart-device approach to assistance with daily tasks and to develop guidelines for user interface for the cognitive assistance device. Specific questions included: Does complexity of the task effect ability to respond? What are the best types of cues to use? What does the system need to sense to provide appropriate cues?
METHOD
 |
Study participants were recruited from local agencies that served seniors with a variety of impairments. Inclusion criteria were score 13-20 on MMSE, and need for supervision, cuing or minimal assistance with self care tasks as rated on the FIM. Fifteen participants were enrolled. Two participants completed trials in their home. Thirteen participants attended day care programs and completed trials at those facilities.
Three self-care tasks were presented to participants. The tasks included: getting and drinking a glass of water; brushing teeth/dentures; and a dressing task in which male participants were asked to don shirts and female participants were asked to don sweaters or jackets. These tasks were selected as they represented common tasks for which seniors with cognitive impairment might require cueing and also because each represented an increasing level of complexity.
 |
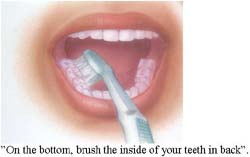
A cuing system was designed that did not require participants to physically interact with the system, but participants were asked follow cues given. A “smart cuing” system was simulated by setting up a wireless camera and speakers or flat monitor in the room with the participant. The camera allowed the researcher to view the performance of the participant on a monitor. The speaker or monitor in the room with the participant were used to deliver the cues. Each task was presented with multiple conditions. The cues to initiate the task were given using the mock smart system. The researcher then observed the performance and determined what cues should be given to correct errors in performance, give more information to guide performance, and answer questions. Cues for the hydration and dressing task were verbal and included both the recorded voice of the investigator and synthesized voice cues. The cues for the oral care task combined verbal and visual cues. A record of cues given and the response was kept for each trial.
RESULTS
 |
In the drink of water task, all participants were able to complete the goal of drinking at least 4-6 oz of water. A mean of 3.18 cues were given per trial; this included the first cue to initiate the task. The remaining cues given in order of mean occurrence were cues with additional information to perform the task, inquiries related to task completion, and repeated cues due to lack of response or hearing difficulties. There were 10 participants in the oral care task. One participant was withdrawn because she could not hear the cues delivered through the monitor speakers. All other participants were able to complete the task of brushing all the surfaces of their teeth. Only two required additional cues. One participant needed an average of 3 extra cues per task, several of which related to safety. The other required 2 additional cues related to a tendency to perseverate in brushing one area. Although a monitor provided visual cues demonstrating the verbal instructions, none of the participants looked at the monitor.
Seven elders with cognitive impairment participated in the dressing task. They were all able to dress appropriately, collars turned down, shirts tucked in and buttons buttoned. In addition to the cue to don the piece of clothing, all participants were given an additional cue to check their appearance in the mirror. Three male participants required additional cues to fix errors such as a collar up in back or shirt not tucked-in, in the back.
DISCUSSION
The results indicate that elders with moderate cognitive impairment respond positively to technologically delivered cues. Cues providing additional information or instruction were needed, however. Further research is is needed to identify individuals who are most likely to require this cuing. It may be possible to successfully cue elders with MMSE cores lower than 13. These encouraging results suggest that development of a genuine smart cueing system would be useful. Investigators have also gained insights as to the hardware and software requirements of such a system such as improved monitor speakers so that persons with moderate hearing impairment could be included.
REFERENCES
- Cummings, J. (1984). Dementia: Definition, classification, and differential diagnosis. Psychiatric Annals, 14, 85–89.
- 2000 Progress report on Alzheimer's disease: Taking the next steps (n.d.). Retrieved July 26, 2001 , from National Institute on Aging Web site: http://www.alzheimers.org/pubs/pr2000.pdf
- Zarit, S.H., Todd, P.A., Zarit, J.M. (1986). Subjective burden of husbands and wives as caregivers: A longitudinal study. Gerontologist, 26 (3), 260-266.
- Pynoos J, & Ohta, R.J. (1991). In-home interventions for persons with Alzheimer's disease and their caregivers. Physical and Occupational Therapy in Geriatrics, 5, 83-92.
- Anthony-Bergstone, C.R., Zarit, S.H., Gatz, M. (1988). Symptoms of psychological distress among caregivers of dementia patients. Psychology and Aging, 3 (3), 245-248.
- Mihailidis, A., Fernie, G., & Cleghorn, W. (2000). The development of a computerized cueing device to help people with dementia to be more independent. Technology and Disability, 13, 23-40.
- Rogers , J., Holm, M., Burgio, L., Granieri, E., Hsu, C., Hardin, M., & McDowell, B. (1999). Improving morning care routines of nursing home residents with dementia. Journal of the American Geriatrics Society, 47, 1049 –1057.
- Rogers , J., Holm, M., Burgio, L., Hsu, C., Hardin, J., & McDowell, B. (2000). Excess disability during morning care in nursing home residents with dementia. International Psychogeriatrics, 12, 267-282.
This is a publication of the Rehabilitation Engineering Research Center on Technology for Successful Aging, which is funded by the National Institute on Disability and Rehabilitation Research of the Department of Education under grant number 3303466-12. The opinions contained in this publication are those of the authors and do not necessarily reflect those of the Department of Education
