Improving Quality of Life: Design of an Automated Pressure Relief Timer for Pressure Sore Prevention
Kate Brizzi, Seetal Erramilli, Mariana Garcia, Mara Modest, Ewelina Styczynska, Kelly Twomey
The Pennsylvania State University Department of Bioengineering, University Park, PA
ABSTRACT
Pressure sore development is a devastating consequence of being wheelchair-bound, but it can easily be prevented through a series of pressure relief exercises. With input from healthcare professionals and patients, an automated pressure relief timer (Auto-PRT) has been developed. Auto-PRT ensures that patients conduct 15 second pressure relieving exercises every 15 minutes. This novel device sends patient-seating information from the cushion to a programmable microchip which, in turn, outputs data to alarms. Robust testing of the design has ensured that the device can accommodate patients weighing between 45.36 – 90.72 kg while allowing for various styles of pressure relief exercises. Prototype testing has firmly established the reliability of the device, with an average exercise time of 15.04 ± 0.54 sec and an average sitting time of 14.99 ± 0.35 min over six continuous hours of trials. The use of Auto-PRT device during pressure relief training will optimize patient independence while assisting in pressure sore prevention.
Keywords:
pressure sores, wheelchair, exercise, pressure relief
BACKGROUND
A pressure sore, also called a decubitis ulcer, is an area of epidermis where the tissue degrades because a patient fails to change positions for extended periods of time. This condition is a critical problem for wheelchair bound patients and health providers, with 2.5 million pressure ulcers treated each year in U.S. acute care facilities alone (1). Unrelieved pressure constricts blood vessels, starving the skin of nutrients and oxygen causing sores on the epidermis. Most often, pressure sores develop where skin covers bony prominences, such as the sacrum and the ischial tuberosities. Pressure sores are a serious problem especially in paraplegics; their nerves are incapable of sending pain or discomfort messages to the brain to prompt a position change (2). When left untreated, pressure sores can progress from a small irritated patch of skin to a variety of serious complications that include bacteremia, osteomyelitis, squamous cell carcinoma and sinus tracts. Recovery requires additional weeks of hospitalization or bed rest to allow the sore(s) to heal; this means an even longer recovery time and time away from home and work.
Fortunately, pressure sores can easily be prevented through a series of pressure relief exercises (2). The exercise of shifting to the left or right every fifteen minutes for fifteen seconds helps the patients to relieve pressure from their sacrum and ischial tuberosities. By developing an automated multi-sensor wheelchair pressure timer that reminds the patient to conduct these exercises, patients can gain increased independence while avoiding dangerous pressure sores. This reduces the responsibility of caretakers and nurses, who in turn have more time for other patients.
METHODOLOGY
Overview
In response to the critical need for regulated pressure sore prevention measures, a novel multi-button wheelchair pressure relief cushion, Auto-PRT has been designed and implemented in test trials. This device utilizes auditory and visual alarms to remind patients to perform 15-second pressure-relief exercises every 15 minutes, as suggested by the Wound Ostomy & Continence Nurses Society’s Provisional Guidelines for Wound Care (3). When used as a teaching tool for wheelchair bound patients, Auto-PRT alleviates the responsibilities of both health care professionals and patients alike.
Design Process
Specifications for the design were established through direct communication with an occupational therapist at HealthSouth Nittany Valley Rehabilitation Hospital (Catherine Donovan, O.T., personal communication, January 31, 2007), circulation of patient needs surveys, and research of related designs. After an assessment of various design ideas, a final design which took in to account the needs of both patients and care givers was selected and implemented.
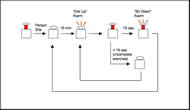
The designed system incorporates 10 push buttons strategically placed to monitor pressure relief of the ischial tuberosities, sacrum, and proximal femur for patients of any size. Information from the push buttons is fed into a programmed PIC 16F877A microchip (Microchip Technologies Inc., Chandler, AZ). This microchip, programmed with a custom-made C++ algorithm, regulates the distribution of information from depressed pushbuttons to timer and alarm mechanisms, as shown in the attached schematic diagram.
A major strength of this computer program lies in its ability to ensure that patients complete the full pressure relief exercise. If the patient does not complete the full 15 second pressure relief exercise, he or she is prompted to continue the exercise until the relief time sums to the mandated 15 second exercise. Furthermore, Auto-PRT accommodates the full range of possible pressure relief exercises, including the complete lift and side-to-side shifting exercises that are commonly prescribed by clinicians
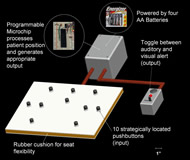
The complete Auto-PRT setup, shown in figure 2, consists of only three major components, allowing it to be easily transported between wheelchairs.
The first component is the cushion itself, which is composed of a 36 cm x 31 cm x 2 cm rubber sheet and 10 momentary switch pushbuttons (RadioShack Corp., Fortworth, TX) encased in a waterproof/incontinence-proof vinyl case. When in use, a ROHO® (The ROHO Group, Belleville, IL, USA) or similar cushion rests on top of this case, eliminating any possibility of abrasions from the pushbuttons themselves. The second component is the battery and microchip box, securely housed in a case strapped to the back of the wheelchair. This placement allows healthcare professionals to easily access the on/off switch while preventing patients from disabling the device during training. Lastly, attached to the front of the wheel chair is the toggle switch/alarm box. The patient is able to use this switch to select the desired alert mode (auditory or visual), depending on his or her environment and personal needs.
DESIGN TESTING AND RESULTS
The following criteria were examined during the testing phase of the design process: consistency of the alarms (both visual and auditory), ability of the system to function under various types of pressure-relief exercises, and the ability of the system to adapt to premature sitting during the exercises.
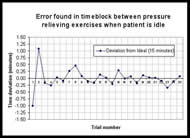
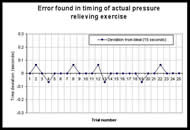
Over six hours of continuous in-chair testing was completed to assess quantitatively and qualitatively the efficacy of each of these criterion. Each trial was defined as one 15-minute timed period followed by a 15-second pressure relief exercise. An alarm was used to indicate the onset of the pressure-relief exercise and to begin timing when it sensed the patient began performing an acceptable exercise. The timer paused if the patient failed to complete the full 15-second exercise and resumed the alarm until a summation of the full 15 seconds was reached.
Twenty-five full trials were carried out, and all executed correctly. To ensure proper execution under any of the three acceptable exercise conditions, 13 full-pressure relief, 6 left partial--pressure relief, and 6 right partial--pressure relief exercises were completed. Of the 25, 12 trials were tested under the condition that the patient sat down too quickly and was thus signaled to resume the exercise. The time summation of intervals that the patient required to adequately complete the exercise was recorded.
The reliability of the Auto-PRT timing is graphed in Figures 3 and 4. Mean time-interval between exercises was 15 ± 0.35 minutes and each pressure relief exercise lasted a mean duration of 15 ± 0.54 seconds. Based on the results, it is asserted with 99% confidence that the alarm will signal the onset of a relief exercise every 15 ± 0.195 minutes and the pressure relief exercise will last 15 ± 0.34 seconds.
CONCLUSION
The Auto-PRT device successfully regulates the timing of pressure relief exercises through the programmable microchip. The design promotes patient independence, allowing users to select the type of alerting mechanism (auditory or visual) and the type of pressure relief exercise. Patient independence and choice is essential since pressure relief exercises must become a lifelong process. Furthermore, increased patient responsibility eases the need for healthcare professionals to monitor patient compliance. In the future, the integrated use of Auto-PRT can improve the patient’s quality of life.
REFERENCES
- Reddy, M., Gill S. S., Rochon, P. A. (2006). Preventing Pressure Ulcers: A Systematic Review. JAMA, 296 (8), 974-984.
- Leher, M. S. (2005). Pressure Ulcers. U.S. National Library of Medicine. Retrieved on February 7, 2007 from http://www.nlm.nih.gov/medlineplus/ency/article/007071.htm.
- Ratliff, C. R. (2005). WOCN’s Evidence-Based Pressure Ulcer Guideline. Advances in Skin and Wound Care, 18 (4), 204-208.
DESIGN TEAM CONTACT INFORMATION
Kate Brizzi (kbrizzi@gmail.com) - 3374 North Hills Road, Murrysville, PA 15668 - 412-417-1418