The Impact of Mattress Types and Bed Inclination on Pressure Injury Prevention
Lindsay Stern1,2, Atena Roshan Fekr1,2
1Institute of Biomedical Engineering, University of Toronto; 2KITE Research Institute, Toronto Rehabilitation Institute, University Health Network
INTRODUCTION
Pressure injuries (PIs) can be defined as injuries to the skin and/or underlying tissue due to prolonged applied pressure and shear forces, typically occurring along the bony prominences of the body [1]. This force can create cellular membrane breakage, initiating a cyclical process of cell death, inflammation, and ischemia [1]. In the Unites States, it is estimated that 3 million adults acquire PIs in the hospital, costing an estimated range between $500-$70,000 USD per patient [2]. In Canada, approximately 26% of patients across all healthcare settings suffer from PIs, costing between $1,247-$597,363 CAD per patient [3] [4]. Furthermore, 15% of elderly patients develop PIs within the first week of stay at the hospital and within the first four weeks of stay in long-term care facilities [3]. However, according to Wounds Canada, approximately 70% of these wounds are preventable [4]. One prevention strategy to alleviate the applied prolonged forces across the body is through the use of therapeutic mattresses, such as reactive and alternating air support surfaces, to assist in reducing the impact of the prolonged pressure and shear forces on the patient [5]. Furthermore, clinical best practice guidelines suggest limiting the Head of Bed (HoB) incline angle to a maximum of 30° to reduce the applied friction and shear forces [6]. However, limited research exists regarding the effects of the therapeutic mattresses at the various HoB incline angles on each part of the body. Therefore, the main purpose of this study is to investigate the impact of a reactive foam mattress and an alternating air support surface regarding pressure alleviation along various segments of the body. Furthermore, this study investigates the effects of four HoB incline angles on each of these mattresses to verify the clinical best practice guidelines. This analysis will provide further insight for clinicians to create more detailed PI care plans to better prevent PIs along all segments of the body.
METHODS
The following sections describe the methodology used for data collection and analysis.

The study took place in a vacant patient room at the Toronto Rehabilitation Institute. The data was collected from the SensingTex pressure mat, composed of 1,056 pressure sensors, with a sampling rate of 1 Hz [5]. The SensingTex pressure mat was placed on top of two mattresses, shown in Figure 1. Figure 1a displays an alternating air mattress, commonly used for patients at high risk of PI development. Figure 1b displays a foam mattress, commonly used for those at lower risk of PI development. This study was approved by the Research Ethics Board at the University Health Network. Informed written consent was obtained by all participants prior to the commencement of the study.
Dataset
Statistical Analysis
The pressure distribution map captured for each participant for each frame was segmented into six portions, which included the full body, the head and neck, the upper torso, the lower torso, the right and left legs, and the right and left feet. Figure 2 illustrates our body segmentation. The mean pressure data for the full body, head/neck, upper torso, and lower torso data were normally distributed, allowing the use of parametric tests, including a paired t-test and a one-way-ANOVA test. However, the mean pressure data for the heels was not normally distributed. Therefore, non-parametric tests were used for this segment analysis, including the Wilcoxon signed-rank test and the Friedman test.
RESULTS AND DISCUSSION
To compare the pressure distribution between the air and foam mattresses, a paired t-test or Wilcoxon signed-rank test was used at each HoB angle. The p-values regarding the mean pressure difference between each mattress can be viewed in Table 1, with a significance threshold set at p = 0.05. The air and foam mattresses are statistically different from each other when considering the full body segment at most HoB angle. However, this finding is not consistent for the other four segmentations. For the upper and lower torso, the head/neck, and heel segments, most of the p-values indicate no statistically significant differences between the two mattress types. This indicates that there is uncertainty that the two mattresses create significantly different mean pressures for these regions.
Table 1. The p-values comparing the mean pressure between the two mattresses at each HoB angle.
| Body Segment | 0° HoB Angle | 10° HoB Angle | 20° HoB Angle | 30° HoB Angle |
|---|---|---|---|---|
| Full Body | 0.0172 | 0.0137 | 0.0116 | 0.0704 |
| Head/Neck | 0.9436 | 0.1986 | 0.1818 | 0.0340 |
| Upper Torso | 0.7252 | 0.9895 | 0.6220 | 0.7208 |
| Lower Torso | 0.2435 | 0.0207 | 0.5723 | 0.8068 |
| Heels | 0.9461 | 0.4903 | 0.7835 | 0.2616 |
To compare the pressure distribution between the HoB angles for the air and foam mattresses, a one-way-ANOVA or a Friedman test were used. Figure 3 displays bar plots of the mean pressure data at each HoB incline angle and their statistical significance between each other for each mattress. The 0° HoB angle was statistically significant compared to the 10°, 20°, and 30° HoB angles for the full body and lower torso segments for both mattresses. This indicates that as the HoB angle increases, the pressure in the lower torso segment increases as expected. This region highlights high risk PI points, particularly at the sacrum and buttocks regions. Therefore, it is important to note that as the HoB incline angle increases, the risk of PI development could increase if the patient is left too long at high HoB incline angles.
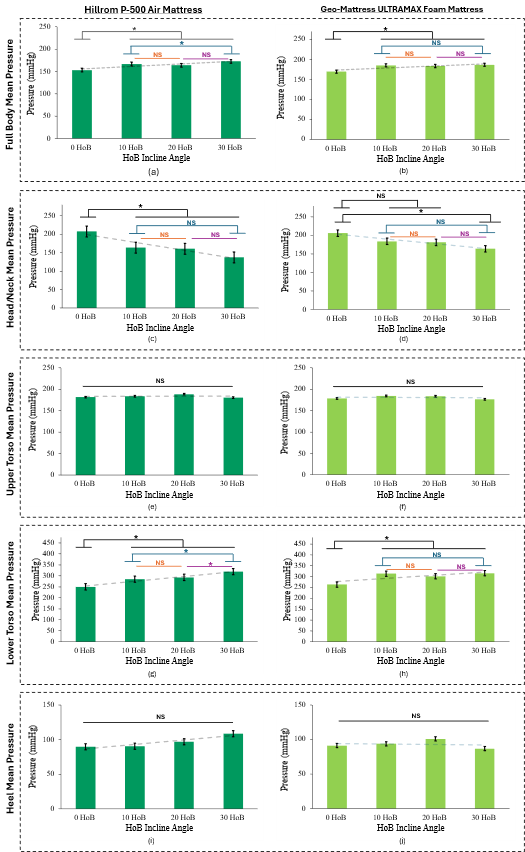
A Tukey HSD or Nemenyi test were used to compare between groups with n=20; * p<0.05; NS: Not Significant.
The head/neck segment for the air mattress was also found to have statistical significance regarding mean pressure between the 0° HoB angle and the 10°, 20°, and 30° HoB angles. However, for the foam mattress, a statistical difference was only discovered between the pressure at the 0° HoB angle and the 30° HoB angles. This highlights that the HoB angle is a critical factor to consider, even at the head/neck region. For the full body, head/neck, and lower torso segments, there is no statistical significance of the mean pressure between the 10° and 20° HoB angles as well as the 20° and 30° HoB angles. This indicates that in some instances a 20° increase in the HoB angle will increase pressure, however, a 10° incremental increase does not significantly impact pressure in these regions. It is important to note that the upper torso and heel segments result in no statistical significance between the mean pressure at any of the angles, indicating that the risk of pressure injury at these regions may be the same, regardless of HoB incline angle.
LIMITATION AND FUTURE WORK
Although there is evidence to support the use of therapeutic mattresses to prevent PI development, to our knowledge, there is no published research regarding the effects of these support surfaces along different segments of the body. Although these results indicate important considerations regarding PI prevention, there were some limitations to the study as well. This analysis was only completed in the supine position with no pillow or blanket use, limiting the generalizability of this analysis. Furthermore, this analysis did not consider the effects of shear, an influential factor regarding PI development. In the future we aim to conduct this analysis in the lateral-lying and prone postures, to evaluate these support surfaces in common sleeping postures. Furthermore, we aim to collect data regarding clinical recommended pillow placement to investigate the effects of these PI prevention techniques. Despite the study's limitations and the need for further research, our analysis of support surfaces and HoB incline angles across five body segments provides valuable insights into the effect of pressure while lying in bed.
CONCLUSION
Therapeutic support surfaces, such as reactive and alternating air support surfaces, create a method to alleviate PI development, with similar pressure alleviation properties. Furthermore, as the HoB incline angle increases, pressure within the full body, head/neck, and lower torso regions increase significantly. These findings have implications regarding PI prevention care plans, allowing a more detailed analysis for PI prevention across the body.
REFERENCES
[1] A. Gefen, ‘The burden of pressure ulcers is one of the most important, yet unsolved, current medical problems. This article reviews the status of technology-based options to prevent pressure ulcers.’, vol. 19, no. 2, 2018.
[2] Z. Moore, S. Gershon, and J. Fletcher, ‘SEM Scanner Made Easy’, Jan. 2018, Accessed: May 27, 2024. [Online]. Available: https://woundsinternational.com/wp-content/uploads/sites/8/2023/02/e2478e8adbc3b45ba778ca23a91396bc.pdf
[3] M. G. Woodbury and P. E. Houghton, ‘Prevalence of pressure ulcers in Canadian healthcare settings’, Ostomy Wound Manage, vol. 50, no. 10, pp. 22–24, 26, 28, 30, 32, 34, 36–38, Oct. 2004.
[4] L. Norton et al., ‘Prevention and Management of Pressure Injuries’, BEST PRACTICE.
[5] E. Haesler, Ed., Prevention and treatment of pressure ulcers/injuries: clinical practice guideline: the international guideline, 3. edition. Prag: Epuap, European Pressure Ulcer Advisory Panel, 2019.
[6] L. Norton et al., ‘Prevention and Management of Pressure Injuries’, BEST PRACTICE.