Feasibility and effectiveness of pre-operative rehabilitation training and education on occupational performance in people with lower limb amputation – a scoping review
Hongwu Wang1, Yuan Li1, Raghu Chandrashekhar1
1University of Florida
ABSTRACT
Lower-limb amputation poses significant challenges, including residual limb pain, phantom limb sensation, and difficulty adapting to post-amputation life, which can reduce the quality of life. Pre-operative rehabilitation training and education have been proposed to enhance post-operative outcomes, but evidence remains limited. This systematic scoping review examines the impact of pre-operative programs on postoperative outcomes for individuals undergoing lower-limb amputation. A search across PubMed, CINAHL, and Web of Science identified studies published between 2014 and 2024. Five studies met the inclusion criteria, demonstrating that pre-operative interventions can improve functional outcomes, reduce hospital stays, and increase prosthetic use. However, the evidence was limited by methodological weaknesses, with studies rated at Levels III and IV and showing moderate to serious risks of bias. While concerns about feasibility persist—such as short pre-surgical timelines and patient comorbidities—the findings suggest pre-operative rehabilitation is both practical and beneficial when integrated into care. Further research is needed to develop standardized, evidence-based protocols accessible across settings. A multidisciplinary approach involving prosthetists and therapists is essential to optimize patient outcomes and support meaningful occupational performance post-amputation.
INTRODUCTION
People with lower limb amputations face many challenges ... Pre-operative training and education may possibly better prepare patients anticipating an amputation for what is ahead of them.
METHODS
Literature search and screening criteria
Three databases were searched during June 2024: PubMed, CINAHL, and Web of Science... Articles not written in English and review articles were excluded from this review.
Literature screening procedure
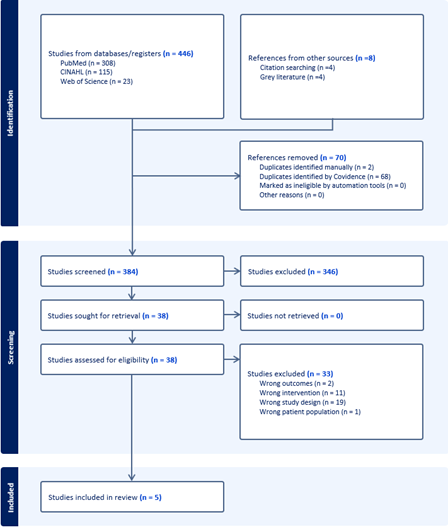
The literature screening process was conducted using the Covidence software... Reasons for exclusion at this phase were recorded.
Data extraction, methodology, rating, and synthesis
Article information was extracted in standard form... Results were tabulated and expanded on from the qualitative data reviewed.
RESULTS
Five studies (Figure 1) were included in the final synthesis ... Matheny et al. (2023) also reported an increased likelihood of receiving a prosthesis if participants engaged in their pre-operative training and education program.
Table 1. The study design and key findings of the five included articles.
| Authors | Year | Design | Key Findings |
|---|---|---|---|
| Bowrey, S., Naylor, H., Russell, P., & Thompson, J. [6] | 2018 | Retrospective Review | Developed the BLARt score to predict functional outcomes in lower limb amputees, aiding preoperative expectations. |
| Daso, G., Chen, A.J., Yeh, S., O'Connell, J.B., Rigberg, D.A., Virgilio, D.C., Gelabert, H.A., Ulloa, J.G. [7] | 2022 | Retrospective Review | Examined ambulatory outcomes and survival in veterans post-lower extremity amputation, with potential improvements noted. |
| Fulton, S., Baird, T., Naik, S., Stiller, K. [8] | 2022 | Retrospective, Matched, Case-Controlled Pilot Service Evaluation | Prehabilitation-plus reduced acute and total hospital length of stay for major lower limb amputation patients. |
| Matheny, H., Woo, K., Siada, S., Qumsiyeh, Y., Aparicio, C., Borashan, C., & O'Banion, L. A. [4] | 2023 | Retrospective matched cohort design | Demonstrated community-wide feasibility of the Lower Extremity Amputation Protocol for vascular amputees. |
| Silva, A. D. M., Furtado, G., Dos Santos, I. P., da Silva, C. B., Caldas, L. R., Bernardes, K. O., & Ferraz, D. D. [5] | 2021 | Longitudinal Study | Showed improved functional capacity in elderly lower-limb amputees after prosthesis rehabilitation. |
Of the five studies, two articles had Level III of evidence... The Bias of the three-level IV studies [6-8] was specified in Table 2.
Table 2. Cochrane Risk of Bias tool of the included Level IV studies
| Domain | Bowrey et al., 2018 [6] | Daso et al., 2022 [7] | Fulton et al., 2022 [8] |
|---|---|---|---|
| Bias due to confounding | Moderate Risk | Moderate Risk | Moderate Risk |
| Bias in the selection of participants for the study | Low Risk | Serious Risk | Low Risk |
| Bias in the measurement of interventions | Low Risk | Low Risk | No Information |
| Bias due to departures from intended interventions | Moderate Risk | No Information | Serious Risk |
| Bias due to missing data | No Information | No Information | No Information |
| Bias in the measurement of outcomes | Low Risk | Low Risk | Low Risk |
| Bias in the selection of the reported result | Low Risk | Moderate Risk | No Information |
DISCUSSION
Our review highlighted the feasibility [4-7] of pre-operation rehabilitation training and the positive impact on postoperative functional outcomes [4-8] in patients with lower limb amputation, even though some healthcare professionals and researchers working with the amputation population were concerned that preoperative rehabilitation was not feasible due to the short time window before surgery, older age, multiple comorbidities, and lack of motivation for behavioral change [8]. This finding agreed with studies in other populations that pre-operative rehabilitation programs are feasible and can be integrated into existing pre-surgical protocols and/or programs [9-11].
The strength of the evidence for using rehabilitation prior to amputation to improve functional outcomes following amputation is low because of the limited evidence and the poor methodological quality rating. More evidence is required to support preoperative rehabilitation for patients receiving lower limb amputation. In addition, no standardized pre-operative programs and/or protocols can be delivered across various settings. A more accessible and evidence-based pre-operation rehabilitation program is needed in future work. Furthermore, prosthetists and therapists, such as occupational and physical therapists, should advocate for a pre-rehabilitative team for patients needing to receive a lower limb amputation to promote occupational performance following the amputation.
REFERENCES
- Hanyu-Deutmeyer, A. A., Cascella M., & Varacallo M. (2024) Phantom limb pain. [Internet]. StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK448188/
- Hijmans, J.M, Dekker, R., & Geertzen, J.H.B. (2020). Pre-operative rehabilitation in lower-limb amputation patients and its effect on post-operative outcomes. Medical Hypotheses. 143:1-9. https://doi.org/10.1016/j.mehy.2020.110134
- Gailey, R., Gaunaurd, I., Raya, M., Kirk-Sanchez, N., Prieto-Sanchez, L.M., Roach, K., (2020). Effectiveness of an evidence-based amputee rehabilitation program: A pilot randomized controlled trial. Physical Therapy. 100(5):773–787. https://doi.org/10.1093/ptj/pzaa008
- Matheny, H., Woo, K., Siada, S., Qumsiyeh, Y., Aparicio, C., Borashan, C., & O'Banion, L. A. (2023). Community-wide feasibility of the Lower Extremity Amputation Protocol amongst vascular amputees. Journal of vascular surgery, 78(4), 1057–1063. https://doi.org/10.1016/j.jvs.2023.06.001
- Silva, A. D. M., Furtado, G., Dos Santos, I. P., da Silva, C. B., Caldas, L. R., Bernardes, K. O., & Ferraz, D. D. (2021). Functional capacity of elderly with lower-limb amputation after prosthesis rehabilitation: a longitudinal study. Disability and rehabilitation. Assistive technology, 16(5), 556–560. https://doi.org/10.1080/17483107.2019.1684581
- Bowrey, S., Naylor, H., Russell, P., & Thompson, J. (2018). Development of a scoring tool (BLARt score) to predict functional outcome in lower limb amputees. Disability and Rehabilitation, 41(19), 2324–2332. https://doi-org.lp.hscl.ufl.edu/10.1080/09638288.2018.1466201
- Daso, G., Chen, A.J., Yeh, S., O'Connell, J.B., Rigberg, D.A., Virgilio, D.C., Gelabert, H.A., Ulloa, J.G. (2022). Lower extremity amputations among veterans: Have ambulatory outcomes and survival improved. Annals of Vascular Surgery, 87:311-320. https://doi.org/10.1016/j.avsg.2022.06.007
- Fulton, S., Baird, T., Naik, S., Stiller, K. (2022). Prehabilitation-plus for patients undergoing major lower limb amputation may reduce acute hospital and total hospital length of stay: A retrospective, matched, case-controlled pilot service evaluation. International Journal of Therapy and Rehabilitation, 29:1741-1645. http://doi.org/10.12968/ijtr.2020.0156
- Carter, H. M., Littlewood, C., Webster, K. E., & Smith, B. E. (2020). The effectiveness of preoperative rehabilitation programmes on postoperative outcomes following anterior cruciate ligament (ACL) reconstruction: a systematic review. BMC musculoskeletal disorders, 21, 1-13.
- Widmer, P., Oesch, P., & Bachmann, S. (2022). Effect of prehabilitation in form of exercise and/or education in patients undergoing total hip arthroplasty on postoperative outcomes—a systematic review. Medicina, 58(6), 742.
- Punnoose, A., Claydon-Mueller, L. S., Weiss, O., Zhang, J., Rushton, A., & Khanduja, V. (2023). Prehabilitation for patients undergoing orthopedic surgery: a systematic review and meta-analysis. JAMA network open, 6(4), e238050-e238050.