The design of a biofidelic mock residual limb for prosthetic socket testing
Clara Phillips1, Aaryan Nagpal2, Fae Azhari1
1Department of Mechanical and Industrial Engineering, University of Toronto; 2Department of Engineering Science, University of Toronto
INTRODUCTION
With the advent of new prosthetic socket materials and designs, rigorous testing is required to ensure these sockets meet clinical requirements and fit properly to a user’s residual limb. To evaluate the effect of socket features on residuum-related clinical outcomes, such as pistoning, suspension, and interfacial stresses, the socket must be used with either a physiological residual limb, or a mock residual limb developed in a lab. Furthermore, adjustable sockets, which are dynamic sockets designed to alleviate significant discomfort caused by daily volume fluctuations of the residual limb [1], [2], must be evaluated with a residuum of varying volume. Most studies evaluating socket performance, including adjustable sockets, rely on clinical testing with patient participants [1]. However, clinical testing demands substantial time and resources, requiring significant changes in participants’ limb volume and accurate measurement of that volume within the socket. Thus, apart from when clinical trials obtain subjective feedback of the socket (e.g., comfort scores or patient questionnaires), using a biofidelic mock limb that replicates both the material composition and volume fluctuations of a physiological limb is more practical than clinical trials, as it reduces costs and allows for a controllable limb volume. While some studies use a static mock limb for bench-top testing of sockets [3], a biofidelic (or, adjustable) limb has not yet been developed.
In this paper, we describe the fabrication of a biofidelic mock residual limb that can adjust in real-time at a controlled rate. We validate the mock limb by measuring its repeatability in changing volume at various rates. While we focus on the application of a biofidelic mock limb for evaluating adjustable sockets, we also discuss adaptations to the design for use for other applications within, and beyond, prosthetics.
METHODS
Design criteria and requirements
Design choices were aimed at creating a mock limb with specifications that closely mimic those of a physiological limb. Volume changes of a physiological residual limb typically occur in the radial direction, at localized regions where there is more soft tissue for fluid displacement. For this study, we examined a transtibial residual limb to select appropriate bladder placement and volume changes. Adjustable transtibial sockets are designed to accommodate localized changes in the posterior compartment, medial tibial flare, and lateral tibial flare. Therefore, it follows that the proposed limb should radially adjust in similar localized areas, i.e., at three axi-symmetric locations around the limb. The proposed biofidelic limb must fluctuate by ±5% in volume, which is consistent with limb fluctuation associated with poor fit [4], thus constituting a meaningful volume change. Diurnal volume fluctuation rates vary significantly depending on factors such as diet and residual limb health [5]. Therefore, the proposed limb should accommodate a wide range of volume change rates from ±0.02%/min to ±10%/min [6].
Design overview and fabrication
The final design comprises three water-filled bladders made from heat-sealed TPU fabric, embedded in a dual-durometer urethane structure. First, the inner core of the limb was cast with VytaFlexTM 60 (shore A hardness 60, Smooth-On, Reynolds Advanced Materials, Chicago, IL) around an aluminum mandrel, to mimic deep harder tissue (Figure 1A). The mandrel was suspended during casting (24 hours) using a clamp. Then, a mold assembly was designed to shape the bladder cavities and form the outer layer of VytaFlexTM 20 (shore A hardness 20, Smooth-On, Reynolds Advanced Materials, Chicago, IL), to mimic softer outer tissue (Figure 1B and 1C). The cured inner core was suspended within the outer shell during casting of the VytaFlexTM 20 (over 24 hours). Lastly, molds were removed, leaving the final dual-durometer urethane limb (Figure 1D), which has a volume of 1,330 mL at its fully-contracted state.
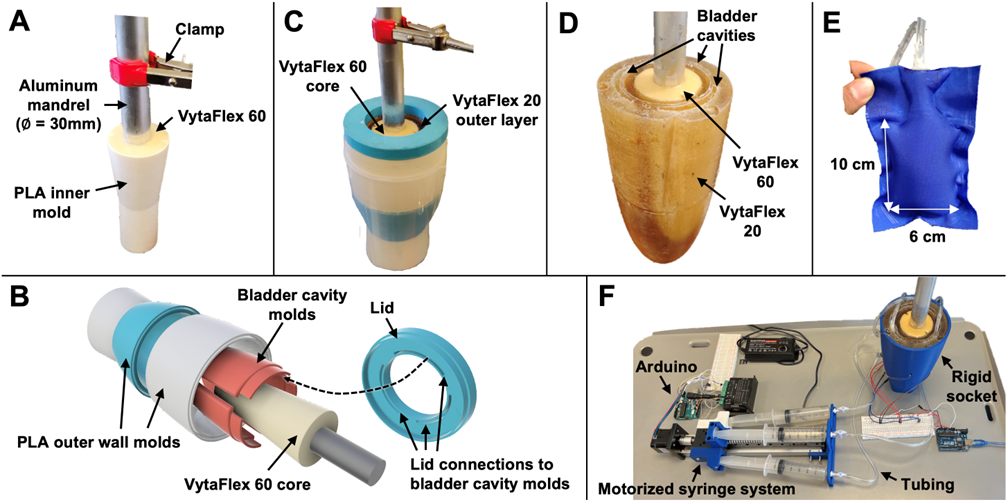
All molds were 3D printed in PLA, sealed to a smooth finish with a thin layer of two-part epoxy, and coated with two layers of UniversalTM Mold Release (Smooth-On, Reynolds Advanced Materials, Chicago, IL). Bladders (Figure 1E) were inserted into the cavities, and their volume of water was controlled by an Arduino-based motorized syringe system (Figure 1F). The F-socket system (Tekscan, Inc., South Boston, MA) was used to measure interfacial pressure between the limb and socket. At full-contraction, the average pressure was approximately 3-5 kPa, which was deemed suitable for a loosely fitted socket [7].
Limb adjustability testing protocol
The biofidelic mock limb was subjected to four different volume change rates inside a rigid socket: a SLOW rate over 24 hours, a MODERATE rate over 3 hours, a FAST rate over 30 minutes, and a VERY FAST rate over 3 minutes. Tests started with the limb at its fully-contracted size, then the limb increased to its fully-expanded size, held, then contracted back to its original volume. The length of the increase, hold and decrease periods were the same: 8 hours, 1 hour, 10 minutes and 1 minute, for the SLOW, MODERATE, FAST and VERY FAST tests, respectively. The limb’s behaviour for different absolute volume changes was tested by performing the SLOW (0.63%/hr), MODERATE (5%/hr), FAST (0.5%/min) and VERY FAST (5%/min) tests from volume changes of -2.5% to +2.5%, and repeating the FAST and VERY FAST tests at double speed from -5% to +5% volume change. Interfacial pressures were measured with the F-socket system to detect the volume change and assess the bladders’ ability to hold their size over these test periods. Given the significant long-term drift associated with the sensors [8], pressures were plotted as a percentage of the maximum pressure reached in each test to allow for comparison between tests.
RESULTS AND DISCUSSION
Effect of volume flow rate on pressure distribution
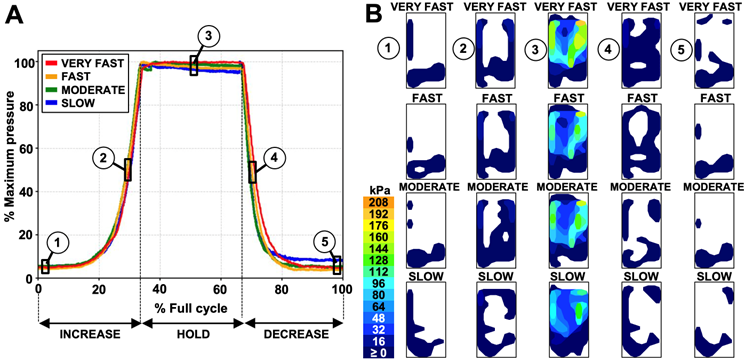
Volume flow rate had little effect on pressure distribution and rate of pressure change throughout the testing cycle. Figure 2A shows similar variation trends in normalized pressure in response to ±2.5% volume change, regardless of whether this change occurred at a SLOW, MODERATE, FAST and VERY FAST rate. Although pressure magnitudes may vary (due to sensor drift), heat maps in Figure 2B show similar pressure distributions among test rates at various stages in the testing cycle, and verify that the distributions are similar during increase and decrease periods of the same test rate. The measured pressure values agree with those of studies measuring interfacial pressure of properly- and tight-fitted sockets [9].
Test repeatability and hysteresis
Tests were repeatable at all flow rates (SLOW was not repeated due to time constraints), varying by a maximum of only about 8% between tests (corresponding to approximately 3-5 kPa) during the hold periods (Figure 3A-C). This variation could be due to different total volumes pumped into the bladders, caused by a slight compliance in the motorized syringe system.
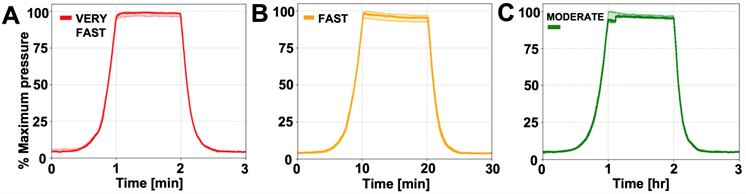
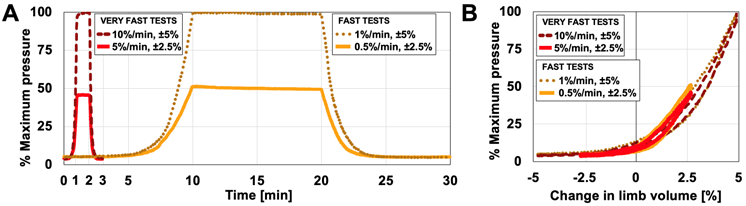
Figure 4A shows a comparison between ±2.5% and ±5% volume changes at VERY FAST and FAST rates. Pressure measurements are normalized with respect to the maximum average pressure reached in the ±5% test. Figure 4B shows similar hysteresis curves between ±2.5% and ±5% tests, thus verifying limb change regardless of start and end volumes. The slight variation in pressure readings between ±2.5% and ±5% tests could be attributed to sensor drift or a slightly different placement of the limb in the socket between tests. The relatively small hysteresis at each test rate is confirmed by the similar pressure distributions shown between points 1 and 5, and points 2 and 4 in Figure 2B.
Applications for use and potential design adaptations
The proposed biofidelic mock limb can be used to evaluate sockets fitted to residual limbs fluctuating in volume up to ±5%. Clinical outcomes (e.g., pistoning and interfacial pressures) can be evaluated by adjusting the size of the limb, rather than swapping out sockets or limbs of different sizes [7], [10]. For adjustable sockets, the proposed mock limb enables the evaluation of the socket’s dynamic mechanism (e.g., straps, buckles, motorized panels [1]) against a fluctuating limb volume in real time.
The biofidelic mock limb may be useful for applications outside of prosthetics. The fit of smart wearables, footwear, compression garments, orthotics, or other assistive devices on a volume-fluctuating limb could be evaluated with the biofidelic limb. The mandrel serves to mimic bone in this design, but it can also be a point of applied load to facilitate testing for any load-bearing applications.
The materials of the dual-durometer urethane limb were selected because their combined material properties and layered structure mimic closely that of a physiological limb. Water was used as the adjustable medium over air for its incompressibility, ease of use, and similar material properties to physiological interstitial fluid or blood [2], but the behaviour of the limb may be adapted as desired by using materials with different material properties (viscosity, compressibility, modulus, etc.).
The placement, shape and size of the bladders also affect the effective material and structural properties of the limb, and can easily be tuned. The deformation of the soft urethane (VytaFlexTM 20) surrounding the bladders is complex, and was not investigated in this study. Nonetheless, we expect that placing the bladders closer to the surface would produce a stiffer limb with a steeper pressure response, especially at smaller volumes. This study characterized the limb behaviour for a specific limb composition and shape; however, if precise material properties of the limb are desired, thorough testing of the effect of bladder placement, bladder size, and anatomical shape of the limb should be performed.
CONCLUSION
Overall, the proposed adjustable mock limb can reliably replicate limb volume fluctuations up to ±5%. The limb is manufacturable with readily available materials and can be adapted for a variety of applications. It allows for controllable bench-top testing during prototyping of adjustable sockets or other devices, eliminating the need for resource-intensive clinical trials, thus bringing devices to clinical use sooner.
REFERENCES
[1] Baldock M et al. Adjustable prosthetic sockets: a systematic review of industrial and research design characteristics and their justifications. J. Neuroeng. Rehabil. 2023 20(1):1–18.
[2] Sanders JE, Fatone S. Residual limb volume change: Systematic review of measurement and management. J. Rehabil. Res. Dev. 2011 48(8):949–986.
[3] Quinlan J, Yohay J, Subramanian V, Poziembo, B, Fatone, S. Using mechanical testing to assess the effect of lower-limb prosthetic socket texturing on longitudinal suspension. PloS one. 2020 15(8).
[4] Fernie GR, Holliday PJ. Volume fluctuations in the residual limbs of lower limb amputees. Arch. Phys. Med. Rehabil. 1982 63(4):162–165.
[5] Sanders JE, Cagle JC, Allyn KJ, Harrison DS, Ciol MA. How do activities walking, standing, and resting influence trans-tibial amputee residual limb fluid volume?. J. Rehabil. Res. Dev. 2014 51(2):201.
[6] Sanders JE et al. Does temporary socket removal affect residual limb fluid volume of trans-tibial amputees?. Prosthet. Orthot. Int. 2016 40(3):320-328.
[7] Karamousadakis M, Porichis A, Ottikkutti S, Chen D. A sensor-based decision support system for transfemoral socket rectification. Sensors. 2021 21(11):3743.
[8] Swanson EC, Weathersby EJ, Cagle JC, Sanders JE. Evaluation of force sensing resistors for the measurement of interface pressures in lower limb prosthetics. J. Biomech. Eng. 2019 141(10):1010091.
[9] Sanders JE, Jacobsen AK, Fergason JR. Effects of fluid insert volume changes on socket pressures and shear stresses: Case studies from two trans-tibial amputee subjects. Prosthet. Orthot. Int. 2006 30(3):257–269.
[10] Seo J et al. A prosthetic socket with active volume compensation for amputated lower limb. Sensors. 2021 21(2):1–17.