MEASURING EARLY INTERVENTION PROVIDER’S USE OF A NOVEL SWITCH-ACCESSIBLE PLAY KIT
Mia E. Hoffman1, Riley Bernas2, Alisha Bose3, Kate Bokowy1, Heather A. Feldner4, Katherine M. Steele1
1Department of Mechanical Engineering, 3Human Centered Design & Engineering, 4Department of Rehabilitation Medicine, 5Center for Research and Education on Accessible Technology and Experiences; University of Washington; 2Deparment of Mechanical Engineering; University of Connecticut
INTRODUCTION
Play is the essence of a young child’s day. Play facilitates cognitive, social-emotional, and physical development [1]. For young children with developmental delays or disabilities, modifications to their toys or environment can greatly support their independent play [2]. One way to facilitate play for children with disabilities are switch-adapted toys – battery-operated electronic toys modified to be activated by an external switch. These toys help children learn cause and effect, expand their play opportunities, and enable them to control aspects of their play environment [3, 4]. However, switch-adapted toys are significantly more expensive than their non-adapted counterparts, available in limited supplies, and may not always be age-appropriate [5].
Beyond toys, augmentative and alternative communication (AAC) systems that can be accessed by either switches or eye-gaze often have built-in games to support learning of the systems and play. However, these devices often are not provided until children are older and cost thousands of dollars or require insurance approval [6]. Other assistive technologies for adaptive play, such as brain-computer interfaces or socially assistive robots, are not yet commercially-available and may not be financially accessible to most children receiving early intervention [7–9].
Young children with developmental delays and disabilities participate in federally-funded early intervention services, which include physical, occupational, and speech therapy. Providers use child-led play as the primary method to engage young children in a “just right challenge” – activities that are engaging without being frustrating [1, 10]. To create an accessible play environment, therapists must consider the child’s positioning and carefully select or adapt toys to match the child’s sensory and motor abilities [1]. Assistive technology has the potential to support independent play in early intervention, but is drastically underutilized [11].
To address this gap in play technologies for young children, our team has developed a novel Switch Kit in conjunction with local families of young children receiving early intervention and their providers. The Switch Kit consists of a MakeyMakey circuit board that is adapted to be switch-accessible and housed within a child-safe container allowing for simple plug-and-play connectivity, an interactive media library created in the Scratch coding language, and a variety of low-cost switches that can be fabricated from household materials (Figure 1). The input device actuates a computer’s arrow keys, space bar, and/or mouse click when a switch is pressed. The Scratch media library included songs that play when a switch was pressed, one-switch options like popping a bubble, two-switch options like making a truck go and stop, and multiple-switch options like playing a piano.
In this paper, we aim to understand how early intervention providers use the Switch Kit in clinical practice by a) quantifying their device usage with clients and b) measuring providers’ perceptions of the Switch Kit.

METHODS
Efficacy of the Switch Kit was evaluated by five early intervention service providers. Providers included one physical therapist (PT), three speech and language pathologists (SLP), and one early intervention teacher. All providers worked in the home environment and worked at different clinics. Providers had an average of 11.8 (RANGE: 5 – 22) years of professional experience. Providers at study entry reported using switch-accessible technology with 5- 30% of their current caseload, which averaged to 2-3 clients for each provider. This study received approval from the Institutional Review Board at the University of Washington. All participating providers gave their informed consent to be included in this research.
Study Design
Each provider was given a complete Switch Kit consisting of an input device and six switches fabricated by the team (Figure 1) to use for 4-6 weeks with clients. As requested, providers were loaned an iPad and/or adapter to be used during the study period. Providers completed a pre- and post- session with the research team. At the initial visit, providers received instruction on how to use the Switch Kit, completed two surveys: a demographic survey and a technology-perception survey, and participated in a short semi-structured interview. At the final visit, providers completed a technology-perception survey again and clinical-implementation surveys, and participated in a longer semi-structured interview on how they utilized the Switch Kit. We purposefully did not set specific parameters for use or dosage recommendations as our goal was to understand how and when early intervention providers chose to incorporate the Switch Kit into their sessions.
Outcome Measures
To evaluate technology perception, providers completed the Quebec User Evaluation of Satisfaction with Assistive Technology: Children’s Version 2.1 (QUEST) at their initial and final visit, using nine technology-focused items on a 1-7 Likert-type scale, where 1 is delight and 7 is terrible [12]. This differs from the traditional QUEST 2.0, which uses a 1-5 scale, with 5 being high. Providers also completed three perceptual implementation surveys: the Acceptability of Intervention Measure (AIM), Intervention Appropriateness Measure (IAM), and Feasibility of Intervention Measure (FIM), each on a 1-5 Likert scale, where 1 is disagree and 5 is completely agree, post-session after using the Switch Kit for 4-6 weeks [13]. Device usage was tracked with a data logger integrated into Scratch games, recording each switch press's date, time, duration, key, and game name. Interaction metrics were calculated using a custom Python script.
RESULTS
Quantifying device usage
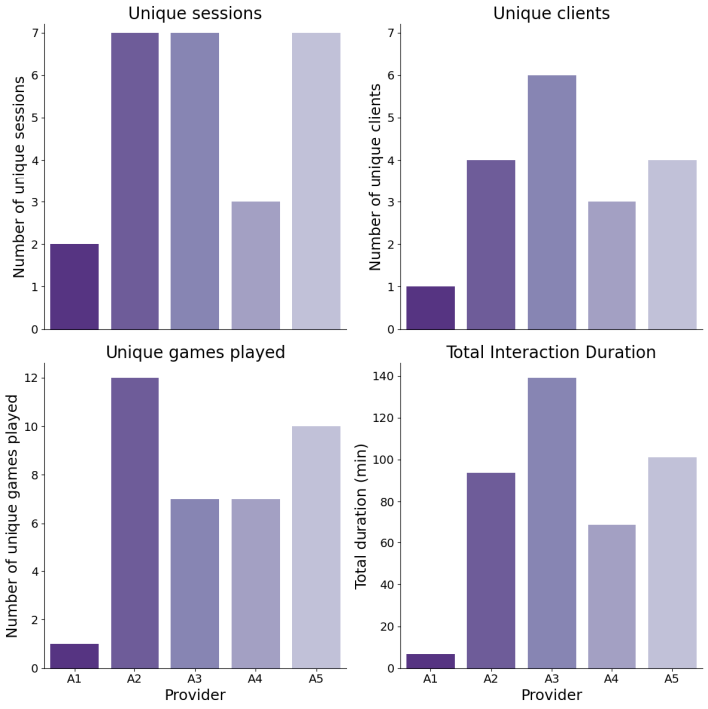
All five providers used the Switch Kit, and their use was successfully logged with in-game metrics (Table 1, Figure 2). Providers used the Switch Kit with 1 – 6 different clients with a range of diagnoses including cerebral palsy, autism spectrum disorder, cortical vision impairment (CVI), and global developmental delay. Providers used the device on average during 5.2 sessions across the entire deployment. However, 4 out of 5 providers used the Switch Kit with the same child more than once. Each provider was provided with 30 different Scratch games to play, providers played on average 2.3 games. Each provider had a different game that they used the most. However, 4 out of 5 providers favored games where there were singular causes and effects, such as pressing a switch and having a bubble pop or having a song play and character dance while the switch was pressed. The game interaction time ranged from 6 seconds to 43.7 minutes (AVE: 15.8 minutes).
Measuring device perceptions
The technology average score of the QUEST at initial visit after learning to use the Switch Kit was
2.25/7 and at final visit after using the Switch Kit for 4-6 weeks was 2.65/7 (Table 2). These scores show an overall positive viewing of the Switch Kit throughout the study (1 = delight). Four out of five providers had a negligible change in their reporting. Provider A4’s outlook on the Switch Kit from a positive view at initial interaction to a more neutral view post-use.
Four out of five providers’ AIM-IAM-FIM scores were ≥ 15/20 (75%, Table 2), indicating a positive view of the Switch Kit as an intervention after using the Switch Kit for 4-6 weeks. Provider A4 reported the lowest acceptability (17/20) and appropriateness (10/20) scores. Both providers A4 and A5 reported the lowest feasibility scores, even though both were still positive (15/20). A4 indicated that the Switch Kit did not seem to be a good match for their clients’ needs, though all other providers identified a positive fit for clients.
|
Interaction Metric |
Provider |
||||
| A1 | A2 | A3 | A4 | A5 | |
| Unique days | 1 | 6 | 5 | 3 | 5 |
| Unique clients | 1 | 4 | 6 | 3 | 4 |
| Number of clients with more than one session | 1 | 2 | 1 | 0 | 3 |
| Unique sessions | 2 | 7 | 7 | 3 | 7 |
| Total Interaction Duration (min) | 6.87 | 93.7 | 139 | 69.0 | 101 |
| Total games played | 2 | 16 | 14 | 12 | 17 |
| Unique games played | 1 | 12 | 7 | 7 | 10 |
| Average number of games played per session | 1.0 | 2.3 | 2.0 | 4.0 | 2.4 |
| Average number of switch presses per session | 36.0 | 207 | 193 | 91.0 | 71.1 |
Table 1. Scratch interaction metrics per provider
|
Provider |
AIM-IAM-FIM Scores (20/20 high) |
QUEST 2.1 (1/7 high) |
|||
| Acceptability | Appropriateness | Feasibility | Pre | Post | |
| A1 | 20 | 19 | 18 | 2.75 | 1.88 |
| A2 | 20 | 20 | 20 | 1.00 | 1.25 |
| A3 | 18 | 17 | 16 | 2.25 | 2.50 |
| A4 | 17 | 10 | 15 | 1.88 | 3.88 |
| A5 | 18 | 16 | 15 | 3.38 | 3.75 |
Table 2. Responses from the QUEST 2.1 and implementation measures surveys
How providers used the Switch Kit
Providers highlighted different ways that using the Switch Kit benefited their clients. For example, A1, an SLP, shared a story of a child who requested more time with the Switch Kit by first signing “more” and then verbalizing “muh.” Another provider, A2, a PT, used the Switch Kit to motivate a child to cruise by moving it around and having the child use their foot to press a switch. However, like any piece of technology, providers experienced problems with the Switch Kit. A4, an early intervention teacher who typically does not work with children with motor delays, found that the Switch Kit was unable to engage two of her clients who were “big movers.” She recounted how one of her clients completely disassembled one of the switches. Additionally, some providers faced technical challenges with the Scratch interface, such as sound issues in their device’s browser or difficulties saving data. Suggestions for improvement included making switches more visually distinct and adding textures for sensory input, using an iPad for easier setup, and adding heavier switches with suction cups for stability. Issues with drooling and mouthing, particularly with the yogurt container switch, were also highlighted.
DISCUSSION
In this work, we showed that five early intervention providers from across several disciplines utilized and valued a novel Switch Kit during client sessions to facilitate access to play. Providers reported that they used the Switch Kit more frequently and with a greater number of clients compared to other switch-adapted toys available to them in their practice settings. Similarly, Clark et al. 2019 found that 5 out of 8 children with complex cerebral palsy under the age of 5 had a higher level of engagement playing with a socially-assisted robot than a switch-adapted toy [8]. Survey results indicated that providers had favorable perceptions of the Switch Kit as a clinical tool for their clients. In this study, providers rated the Switch Kit more positively on the QUEST than speech-language pathologists did after using a socially assistive robot with children aged 6-12 years for eight weeks [14]. QUEST scores for a gaze- based assistive technology platform were similarly favorable to those in this study, as reported by parents of children with severe physical impairments who used the intervention during daily activities for 9-10 months [15].
Many providers used the Switch Kit with children with CVI or other vision challenges. The Switch Kit is beneficial for kids with CVI as tablets provides brightness, and Scratch media can be tailored for high contrast with audio and visual feedback [16]. One DIY switch uses aluminum foil for a shiny surface, making it easier for children with CVI to spot. Other switches can be modified to be visually distinct by adding bright red tape or stickers. A similar project developed a modifiable toy kit for therapists to add light, haptic, or sound feedback to toys; but it was never was open-sourced or commercialized, making it unusable [17].
This study has several limitations. First, Scratch interaction metrics were not always logged due to manual data saving issues reported by providers. They accessed Scratch games using various devices, including iPads and laptops, with mixed feedback: some found laptops easier, while others found them distracting, and some reported sound issues on iPads. As a pilot study, a limited number of providers were involved. A larger study with more providers across a broader area would offer more representative insights. Lastly, introducing technology without leaving it in the home is atypical for early intervention, which usually involves using materials available in the home [18]. Future research should involve leaving the device in families' homes and tracking usage and caregiver perceptions over time.
CONCLUSIONS
All early intervention providers in this study utilized the Switch Kit and expressed enthusiasm about continuing its use with clients. They initially perceived the device as a “mid-tech” solution beneficial for supporting cause-and-
effect learning and developing key skills that can aid future AAC use. As with any technology, experiences varied; one provider found it unsuitable for clients who are not typically switch users. Overall, the Switch Kit represents a low-cost, open-source technology that can help integrate assistive technology into early intervention, an area currently limited in technological use.
REFERENCES
-
Fiss AL, Håkstad RB, Looper J, et al. Embedding Play to Enrich Physical Therapy. Behav Sci 2023; 13: 440.
-
Hsieh H-C. Effects of ordinary and adaptive toys on pre-school children with developmental disabilities. Res Dev Disabil 2008; 29: 459–466.
-
Burkhart L. Stepping Stones to Switch Access. Perspect ASHA Spec Interest Groups 2018; 3: 33–44.
-
Schaefer JM, Andzik NR. Switch on the Learning: Teaching Students With Significant Disabilities to Use Switches. Teach Except Child 2016; 48: 204–212.
-
Rasmussen KM, Chole DM, Hughes R, et al. Caregiver‐reported impact of access to switch‐adapted toys on play for children with complex medical conditions. Child Care Health Dev 2023; 49: 955–960.
-
Lorang E, Maltman N, Venker C, et al. Speech-language pathologists’ practices in augmentative and
alternative communication during early intervention. Augment Altern Commun 2022; 38: 41–52.
-
Siu C, Aoude M, Andersen J, et al. The lived experiences of play and the perspectives of disabled children and their parents surrounding brain-computer interfaces. Disabil Rehabil Assist Technol 2024; 0: 1–10.
-
Clark C, Sliker L, Sandstrum J, et al. Development and Preliminary Investigation of a Semiautonomous Socially Assistive Robot (SAR) Designed to Elicit Communication, Motor Skills, Emotion, and Visual Regard (Engagement) from Young Children with Complex Cerebral Palsy: A Pilot Comparative Trial. Adv Hum- Comput Interact 2019; 2019: e2614060.
-
Blankenship MM, Bodine C. Socially Assistive Robots for Children With Cerebral Palsy: A Meta-Analysis.
IEEE Trans Med Robot Bionics 2021; 3: 21–30.
-
Harbourne RT, Dusing SC, Lobo MA, et al. START-Play Physical Therapy Intervention Impacts Motor and Cognitive Outcomes in Infants With Neuromotor Disorders: A Multisite Randomized Clinical Trial. Phys Ther 2021; 101: pzaa232.
-
Baker FS. Engaging in Play through Assistive Technology: Closing Gaps in Research and Practice for Infants and Toddlers with Disabilities. Gamification: Concepts, Methodologies, Tools, and Applications 2015; 1097–1112.
-
Murchland S, Kernot J, Parkyn H. Children’s Satisfaction With Assistive Technology Solutions for Schoolwork Using the QUEST 2.1: Children’s Version. Assist Technol 2011; 23: 162–176.
-
Weiner BJ, Lewis CC, Stanick C, et al. Psychometric assessment of three newly developed implementation outcome measures. Implement Sci 2017; 12: 108.
-
Spitale M, Silleresi S, Garzotto F, et al. Using Socially Assistive Robots in Speech-Language Therapy for Children with Language Impairments. Int J Soc Robot 2023; 15: 1525–1542.
-
Borgestig M, Sandqvist J, Ahlsten G, et al. Gaze-based assistive technology in daily activities in children with severe physical impairments–An intervention study. Dev Neurorehabilitation 2017; 20: 129–141.
-
Smolansky A, Yang M, Azenkot S. Towards Designing Digital Learning Tools for Students with Cortical/Cerebral Visual Impairments: Leveraging Insights from Teachers of the Visually Impaired. In: Proceedings of the 26th International ACM SIGACCESS Conference on Computers and Accessibility. New York, NY, USA: Association for Computing Machinery, pp. 1–18.
-
Güldenpfennig F, Fikar P, Ganhör R. Interactive and Open-Ended Sensory Toys: Designing with Therapists and Children for Tangible and Visual Interaction. In: Proceedings of the Twelfth International Conference on Tangible, Embedded, and Embodied Interaction. New York, NY, USA: Association for Computing Machinery, pp. 451–459.
-
Williams CS, Ostrosky MM. What About MY TOYS? Common Questions About Using a Bagless Approach in Early Intervention. Young Except Child 2020; 23: 76–86.