Assessing women Veterans’ satisfaction with their current mobility assistive technology
Jessica Stanley1,3; Diya Kad1; Rutuja Kulkarni1; Alicia M. Koontz1,2
1Human Engineering Research Laboratories, VA Pittsburgh HealthCare System
2Department of Physical Medicine and Rehabilitation, University of Pittsburgh
3Department of Public Health, University of Maryland
INTRODUCTION
Around 2 million Veterans in the United States are women, and it is predicted that the female Veteran population will continue to grow in the next twenty-five years despite decreasing Veteran populations [1]. Additionally, more than 50,000 female Veterans have registered into the VA healthcare system in the past year [2]. Historically, VA health services have not provided comprehensive, gender-specific care for female Veterans due to the low rates of female matriculation into the armed services [3]. Current healthcare practices aim to develop assistive technology that reflects the mobility needs of these women, but often fall short of providing customizable, unique devices that promote healthy and effective living. Little is known about the concerns of women Veterans regarding their mobility devices. Previous research studies that analyzed Veteran needs provide insight into predominantly male populations. The changing Veteran population demands reformed healthcare practices that provide mobility devices unique to the user, consistent with the priorities of female Veterans. This cross-sectional, exploratory research study aims to understand the concerns of female Veterans regarding satisfaction with their current mobility assistive technology in meeting their general needs and related services. A second objective was to explore differences in satisfaction across device types.
METHODS
Participants
Participants from the study were identified from a list of female Veterans who had received a mobility device from the VA healthcare system in the past five years using the VA National Corporate Data Warehouse and VA’s Spinal Cord Injury Registry. Participants were invited to participate in a national anonymous survey from May of 2021 to April 2022. Out of approximately 4000 eligible women, 700 women completed the survey. This study was approved by the Institutional Review Boards at VA Pittsburgh Healthcare System and the Edward Hines, Jr. VA Hospital. Respondents provided informed consent for their participation in this study.
Experimental Protocol
This study analyzed a sub-component of an online survey designed to assess female Veterans’ needs regarding their mobility device within three primary areas: satisfaction with their mobility device and procurement, functional mobility, and the psychosocial impact of their device. Respondents also were asked to answer questions on their demographics. The Quebec User Evaluation Satisfaction on Assistive Technology (QUEST) was the focus of this study and was utilized to assess the Veterans’ satisfaction with their primary mobility device. The QUEST is a validated and reliable clinical instrument containing two subscales: Device and Service. Each subscale presents unique satisfaction items that are rated based on a general Likert scale (1: Not satisfied at all – 5: Very Satisfied). Satisfaction areas of the QUEST include dimensions, weight, adjustability, durability, easy usage, comfort, and effectiveness of their device. Service-level items include service delivery, maintenance, professional, and follow-up services. If respondents rated any satisfaction item a 4 or lower, they were provided a comment field. The QUEST also asks respondents to rank their top three most important satisfaction items.
Analysis
Descriptive statistics were determined for the QUEST as well as the demographical data (SPSS Version 28). An average QUEST score was calculated over all the items and for each subscale (Device and Service). Frequencies and percentages were used to describe the ranking portion of the QUEST. A one-way ANOVA test was used to assess differences in QUEST items and overall scores by primary device group. The qualitative portion of the survey was evaluated using inductive thematic analysis through NVIVO Version 14 [4]. With representative codes reflecting the comments of the respondents, this data underwent a process of synthesis and consensus building with three researchers to determine the grouping of the codes and the overarching themes. All data were sorted by primary device type for analysis.
RESULTS

Participants: 571 respondents had sufficient data for quantitative analysis (completed at least 75% or more of the QUEST) and 446 of these respondents left comments for qualitative analysis. Respondents represented a diverse population with ages ranging from 18 to 80+ with 85.3% of respondents between the ages of 50 and 80+. Respondents were diagnosed on average 11 ± 5 years ago with their disability with the three most commonly reported being: Multiple Sclerosis: 16.5%, Spinal Cord Injury (SCI): 8.9%, and Osteoarthritic/Rheumatoid Arthritis: 8.1%. Approximately 50% of respondents reported having more than one disability.
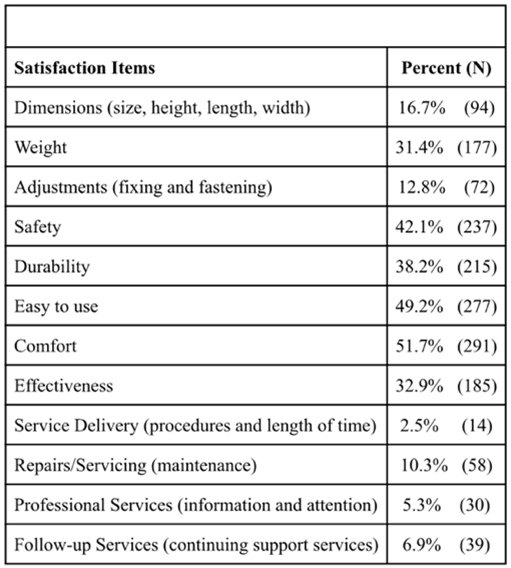
Quantitative Analysis: QUEST scores showed high levels of satisfaction overall (Table 1). There were no differences in the overall satisfaction scores between device groups. However, there was a statistically significant main effect with the dimension satisfaction item. A Post Hoc test showed that power wheelchair users had higher satisfaction with their dimensions compared to leg/foot orthotic users (p=0.01). The most important satisfaction factors reported were comfort (51.7%), easy to use (49.2%), safety (42.1%), durability (38.2%), effectiveness (32.9%) and weight (31.4%) (Table 2).
Qualitative Analysis: Four main themes were consistent across all device categories: equipment issues, physical and psychological impact of device, unmet service needs and usability issues. The majority of concerns were focused around equipment issues (42% of comments) followed by unmet service needs (28.1%), physical and psychological impact of device (14.7%) and usability issues (14.0%). There were three sub-themes under equipment issues which were also prevalent among all device types: issues with mechanical design, lack of features or customizability, and poor-quality components/material. Four sub-themes under the unmet service needs that were present among all device types with the exception of crutch users (possibly due to the small sample size/number of comments) were: lack of efficiency, lack of quality, issues with service providers, and lack of access. A fifth sub-theme under unmet service needs for the scooter group was user barriers to access. The following sections describe the results of the thematic analysis by device.
Canes: User concerns emphasized issues with the ‘Mechanical Design’ theme (20%). Due to poor support, awkward use, inadequate weight, and little to no adjustability, canes fail to complete the objective they were manufactured to do. Users also felt that the device ‘Lacks Features or Customizability’ that are desired to feel secure (11%).
“Canes are slippery on ice and can make falling worse. Also, high winds can blow a cane while walking with it making it more difficult to control.”
Around 18% of concerns reflected a ‘Physical and Psychological Impact of the Device’, with canes causing pain, discomfort, and poor posture for users.
Walkers: Users communicate strong discontent with the ‘Mechanical Design’ of their device (25.7%). Issues with size, adjustability, and utilization affect the usability of the device, limiting the independence of the user, and affecting the ADLs that the device is manufactured to successfully do. Concerns reveal critical barriers to “Usability” in varying manufacturing, public or crowded areas (18.1%).
“Plastic knobs to adjust height are hard for someone with grasping issues to hold onto. The knobs loosen constantly making the handles wobble.”
Under the service theme some female Veterans were left with poor service experiences, leaving their concerns unheard, unaddressed and their repairs incomplete (21.1%).
“Need more mechanics, maybe a real female one. She would know about the issues.”
Leg or Foot Orthotic: Respondents offered concerns predominantly about ‘Mechanical Design’ (23%) followed by ‘Physical and Emotional Impact of the Device’. Undesired weight, little adjustability, and male-oriented designs make users feel that their needs are often overlooked.
“They send me an orthopedic insert for males versus females. I only received female
inserts once. I have very narrow feet.”
Despite their device being manufactured to improve mobility and pain, responses demonstrate the severe negative impact of the device, which often outweighed the aid their device provided (17.2%). Beyond causing pain, strain and discomfort to the user, they also communicated that their device was tiring to use, inconvenient, and generally created more detrimental consequences for the user.
“It’s humiliating and demeaning. It diminishes my sense of independence and self-pride.”
Manual Wheelchair: Manual wheelchair users communicated concerns about the ‘Mechanical Design’ (26.1%) including how the device is manufactured with limited to no adjustability, an incompatibility with other necessary mobility equipment, and undesired size and weight. The dimensions and components not only cause pain and discomfort, but negatively affect the respondent’s psychosocial well-being (12.3%). Responses note that the device itself is not usable (14%). It is difficult to transport to other places, incompatible with varying terrains, and generally difficult to use for long periods without hindered independence.
“It does not give me the independence I need in a mobility device. I’m reliant on my husband, or another person, for help to get me where I need to go.”
Power Wheelchair: Users expressed discontent with the mechanical design of their device (26.9%) due to its bulky and cumbersome frame. Users find it difficult to utilize the functions it was designed to allow. Additionally, users communicate that the device only worsens or creates more medical conditions (15.5%).
“Positioning is critical. I have a particular problem with the seat being in contact with my lady parts all day. A seat specifically designed for a woman’s anatomy would be very helpful.”
Concerns highlighted barriers to the usability of their device (16.5%). Users find it difficult to utilize their device in varying conditions. Additionally, due to its manufacturing, transfer, transport, and manually moving the device often transforms a typical task into a daily struggle. Regarding service, women commented that they felt alienated, ignored, and dismissed in clinical settings.
“Because women Veterans are put on the low priority lists, being told ‘well you can contact you congressman if you do not like it’. Or they tell those of us who are 100% service connected, use your own Insurance, knowing that we do not get reimbursed for out-of-pocket expenses.”
Scooters: Scooter users communicate high levels of dissatisfaction for the ‘mechanical design’ of their device and its ‘Usability’ (31.8%). Users expressed dissatisfaction with it’s shape and size, and were frustrated with it’s adjustability. Scooters lack customization, which leads to ill-fitted, suboptimal products. Scooter’s difficult features negatively affect users and hinder their ability to perform activities of daily living. Users highlight the difficult usability of their device, which affects travel, duration in their device, and independence (17.5%).
“I live out in the country. The school is a 3 wheeled scooter. Is extremely unstable on bumpy terrain. I haven’t been on my lawn since I’ve gotten a scooter.”
Regarding “Unmet Service Needs” scooter users find themselves with little to no maintenance or follow up resources, poor service delivery, and inconvenient servicing (13%).
Crutches: Respondents mainly had issues with ‘Mechanical Design’ (28.6%) and the ‘Physical and Psychological Impact’ of the (23.8%). Due to poor mechanical design, users often suffer both discomfort and pain, which in
turn affects the usability of the product. Limited to no adjustability or collapsibility present critical barriers to mobility for crutch users.
“It makes it uncomfortable, and a few times unsafe because it wasn’t grabbing my arm, and I managed to fall when I let go of the handle.”
DISCUSSION
The female Veterans in this study overall reported high levels of satisfaction with their mobility devices and there were no differences among primary devices except for the dimension satisfaction item. Leg/foot orthotic users reported lower levels of satisfaction in this item compared to power wheelchair users. From the comments women described their brace/orthotic as being too bulky, sized for males only, and were ill-fitted to their body. While similar comments were received for power wheelchair users, an ill-dimensioned orthotic/brace may have a greater impact on functional mobility than a bulky/ill-fitted wheelchair [5]. Female Veterans across all primary device types express discontent under several themes. A majority of comments seem to focus on mechanical design. Equipment issues were associated with usability issues and negative psychosocial impacts. Frequent concerns about mechanical design and usability emphasize that current practices fail to manufacture or provide devices with an end-user feedback approach in mind. The prevalence of significant service concerns in all device type groups emphasize the crucial call for reforming clinical services with regards to improving provider training and customer relations, timeliness of services and improved access to maintenance, repair and follow-up services. Concerns regarding gender-specific care demonstrate barriers to the functionality of female Veteran devices and the mobility of these women. There is significant potential and need for the improvement of gender specific manufacturing and procurement of mobility devices.
Limitations
The open-ended feedback provided on the QUEST does not reflect the manner at which these respondents quantitatively rated the satisfaction items. Respondents who communicated dire concerns about the functionality of their device, simultaneously rated the same corresponding satisfaction items high on the Likert scale. As a result, it is probable that the QUEST scores do not adequate reflect their dissatisfaction with their device and services. By including only women who have obtained a mobility device in the last five years from the VA, the design limits how applicable these results are to the general population of female Veterans. During the inductive coding process, despite instructions, many women commented on devices other than the ones they stated as their primary device and it was sometimes difficult to tell what type of device they were referring to.
Conclusion
This study demonstrates that despite a significant portion of female Veterans quantitatively ranking each satisfaction item quite high, qualitative data continues to show a significant level of dissatisfaction for their device and its usability, as well as the services obtained during the provision and follow-up process. These findings present critical demands for improvement in both the devices administered by the VA and the services offered through the system. Mobility devices should reflect an end-user feedback approach to manufacturing, while services should demonstrate a strong commitment to improving provider interactions and quality and timeliness of the services. The data in this study highlight which areas to begin to focus improvements.
REFERENCES
-
VetPop2020: A Brief Description What’s New. (n.d.).
https://www.va.gov/vetdata/docs/Demographics/New_Vetpop_Model/VetPop2020_A_Brief_Description.pdf -
Department of Veteran Affairs. (2024). More than 50,000 women veterans enrolled in VA health care over past 365 days, marking the largest enrollment year ever for women veterans. VA News. https://news.va.gov/press-room/50k-women-veterans-enrolled-in-va-healthcare-over-past-365-day/
-
Sheahan, K. L., Goldstein, K. M., Than, C. T., Bean-Mayberry, B., Chanfreau, C. C., Gerber, M. R., Rose, D. E., Brunner, J., Canelo, I. A., Darling MSHS, J. E., Haskell, S., Hamilton, A. B., & Yano, E. M. (2022). Women Veterans’ Healthcare Needs, Utilization, and Preferences in Veterans Affairs Primary Care Settings. Journal of General Internal Medicine, 37(S3), 791–798. https://doi.org/10.1007/s11606-022-07585-3
-
Naeem, M., Ozuem, W., Howell, K. E., & Ranfagni, S. (2023). A step-by-step process of thematic analysis to develop a conceptual model in qualitative research. International Journal of Qualitative Methods, 22(1), 1–18. Sagepub. https://doi.org/10.1177/16094069231205789
-
Faieta, J., Schmeler, M. R., Schiappa, V. J., Hand, B. N., Schein, R. M., Saptono, A., Berner, T., & DiGiovine, C. P. (2019). Evaluation of Service Delivery Effectiveness Through Patient-Reported Outcome Measures. American journal of physical medicine & rehabilitation, 98(12), 1072–1078. https://doi.org/10.1097/PHM.0000000000001245
ACKNOWLEGEMENTS
This work was supported by a SPIRE Award # RX003452-01A1 from the United States Department of VA RR&D Service, NSF ASPIRE REU Grant #2149772 and VA Center Grant #B2988-C.