Kaitlin M. DiGiovine![]() 1
1![]() , Stephanie K. Rigot, DPT
, Stephanie K. Rigot, DPT ![]() 2
2![]() , Lynn A. Worobey, PhD, DPT, ATP
, Lynn A. Worobey, PhD, DPT, ATP![]() 2,3,4
2,3,4![]()
University of Pittsburgh Departments of ![]() 1
1![]() Health and Rehabilitation Sciences,
Health and Rehabilitation Sciences, ![]() 2
2![]() Bioengineering,
Bioengineering, ![]() 3
3![]() Physical Medicine and Rehabilitation,
Physical Medicine and Rehabilitation, ![]() 4
4![]() Physical Therapy
Physical Therapy
INTRODUCTION
Up to 81% of individuals with spinal cord injuries (SCI) report experiencing pain. [1] Negative consequences secondary to pain among individuals with SCI include worse health and mood, and lower satisfaction with life and quality of life (QOL) scores. [1,2]After SCI, individuals who ambulate after a SCI often have lower pain severity, and higher satisfaction with life and quality of life scores.[2,3] However, individuals who require assistance from others, assistive devices to ambulate, or transition mode of mobility from ambulation to wheelchair have a decrease in QOL and satisfaction with life scores and an increase in pain severity. [2-4] While studies have evaluated pain severity over time, they have not controlled for other variables besides mode of mobility.[2,3]. Also, previous studies did not evaluate when the mobility transition occurred and participants varied at each timepoint, this is remediated in the present study[2].
This study builds upon past work to investigate changes based on mode of mobility, up to 10 years after injury with the inclusion of matched pairs controlling for sex, age, lower extremity motor score (LEMS) and upper extremity motor score (UEMS) at discharge to investigate the relationship between mode of mobility and pain while minimizing the effect of other covariates. We hypothesized that at 1-year individuals who use a wheelchair will experience more pain severity and pain interference than their ambulatory matched pairs. Additionally, we hypothesized that individuals who changed their mode of mobility from ambulation to wheelchair use would experience more pain severity and pain interference than individuals who go from ambulation to wheelchair use or those who do not change mobility type.
METHODS
Participants
Data was collected from the National Spinal Cord Injury Database (NSCID) which contains information from people who present with a traumatic SCI to one of the SCI Model Systems. Individuals were included if they had 1-, 5-, and 10-year time points for mode of mobility, pain severity and pain interference. Participants self-reported their primary mode of mobility at 1-, 5- and 10-years.
Matched Pairs
Individuals who ambulate and wheelchair users were matched at 1-year based upon the following factors that are known to influence mobility and/or pain: sex, age (± 5y), LEMS at discharge (±3), and UEMS at discharge (±5). By matching these factors, any differences in pain severity and interference, are more likely to be due to mobility group. After 1-year, individuals were able to transition mode of mobility and pairs of ambulators and wheelchair users may not have been maintained over time.
Mobility Group
To analyze primary mode of mobility transitions between 1-year, 5-years, and 10-years respectively, individuals were divided into the following groups: ambulatory, ambulatory, ambulatory (AAA); wheelchair, wheelchair, wheelchair (WWW); ambulatory wheelchair, wheelchair (AWW); wheelchair, ambulatory, ambulatory (WAA); ambulatory, ambulatory, wheelchair (AAW), wheelchair, wheelchair, ambulatory (WWA); wheelchair, ambulatory, wheelchair (WAW); ambulatory, wheelchair, ambulatory (AWA). For statistical purposes, groups with less than 10 individuals were excluded: WWA, AAW, WAW, and AWA.
Pain Severity and Pain Interference
Pain severity was assessed by asking: "Using a 0-10 scale with 10 being pain so severe you could not stand it and, 0 being no pain, what has been the usual level of pain over the past 4 weeks?" Of the individuals who reported having pain, pain interference was assessed with the question: "During the past 4 weeks, how much did pain interfere with your normal work including both work outside the home and housework (or usual activities)? 0 Not at all, 1 A little bit, 2 Moderately, 3 Quite a bit, 4 Extremely." For this study, this variable was categorized by "no pain interference" (score of 0); "mild pain interference" (score of 1-2); or "severe pain interference" (score of 3-4). If an individual reported no pain severity, they were not asked to report their pain interference as to avoid double counting individuals
Data Analysis
Data analysis was conducted using IBM SPSS Statistics version 27.0. Descriptive statistics were calculated for demographics and between group differences using paired t-tests for continuous variables and chi-square for categorical variables. A paired t-test and chi-square test was conducted to assess differences between pain severity of matched groups and differences between pain interference of matched group at one year, respectively.
A two-way repeated measures ANOVA was used to determine the effects of mobility group and time on pain severity. Chi-square analysis was conducted for each mobility group comparing time and level of pain interference. Linear regressions were conducted to analyze the effects of mobility group and change in pain interference (decrease, no change, increase) on change in pain severity between 1-5 years and 5-10 years, with those who increase in pain interference being the reference.
RESULTS
Participants
Of the 252 (126 matched pairs) people in this study, 216 (85.7%) were male, with an average age at injury of 39.67 ± 14.24, average LEMS and UEMS at discharge of 21.44 ± 15.34 and 39.91± 12.88, respectively. There were no differences between groups based on race or injury level with 69.40% white and 55.0% with paraplegia. Only 110 ambulators and 101 wheelchair users reported pain severity>0 at one year and therefore only those individuals were asked to report their pain interference.
Pain severity at 1 year and over time
At one year, there were no significant differences in pain severity between matched pairs in the ambulatory and wheelchair groups (p=0.64). There was also no change in pain severity overtime (p=0.12) nor any difference in pain severity within or between mobility trajectory groups (p=0.56, p=0.58).
Pain interference at 1 year and over time
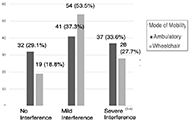
At one year, the difference between pain interference based on mode of mobility trended toward significance (x2=5.97, p=0.05, Figure 1). A greater proportion of wheelchair users experience mild pain interference as compared to individuals who were ambulatory, for whom pain interference was more evenly distributed among the three groups.

There are no significant differences between mobility groups over time in pain interference (x2=3.23, p=0.344) (Figure 2). There are relatively few individuals who change pain interference over time in the groups where no mobility transition occurs (AAA and WWW). The AWW group decreases in the number of individuals with severe pain interference and increases the number of people with mild pain interference. In contrast, the WAA group increases the number of people with severe pain interference and decreases the number of people with mild pain interference.
Pain Severity vs Pain Interference

Between 1 year and 5 years, change in pain interference is a significant predictor of change in pain severity (p<0.001), independent of mode of mobility trajectory (Figure 3a). As pain interference decreases, pain severity significantly decreases as compared to the reference group (B= -2.07, p<0.001). If an individual's pain interference remains the same between 1 and 5 years, their pain severity decreases by a lesser amount as compared to the reference group (B= -0.75, p= 0.045). These relationships were not retained between 5 and 10 years where despite decreases in pain interference there were increases in pain severity among those in the AAA and WWW (p=0.14) (Figure 3b).
DISCUSSION
There were no differences in pain severity between those who ambulate and those who use a wheelchair at 1- year. Because pairs were matched, we can conclude that there may be additional factors, besides primary mode of mobility that affects pain severity, such as type of pain or level of injury (tetraplegia or paraplegia).[1] Over time, there were not differences in pain severity based on mobility group. This is in contrast to previous studies which found higher levels of pain among individuals who transitioned from ambulation to wheelchair.[2,3] This difference may be because the aforementioned studies analyzed transitions occurring after discharge from inpatient rehab while the present study examines mobility changes only after one year following the injury.[2,3] This could indicate the earlier the transition occurs the more impactful it is on pain severity. This also fails to support the original hypothesis predicting that individuals using a wheelchair at one year would experience more severe pain.
Between 1- and 5-years, an individual's change in pain interference significantly predicts their change in pain severity; however, this significance disappears between 5 and 10 years. For individuals who did not change their mode of mobility (AAA, WWW) median pain severity is relatively constant across levels of pain interference overtime. This is in contrast to the AWW and WAA groups which show a more linear relationship between change in pain interference and change in pain severity between 1 and 5 years; however, this trend disappears between 5 and 10 years. This could suggest that over time individuals whose mode of mobility is constant become better at managing their pain and therefore regardless of pain severity, their pain does not interfere as much with their life.[10] In addition, individuals who continue to use the same mode of mobility may see a decrease in pain interference due to an improvement in their mobility technique with additional training and practice.[11]
STUDY LIMITATIONS
Due to the small sample size of individuals who made multiple mobility aid transitions (AWA or WAW) and individuals who made a mobility transition between 5 and 10 years (AAW or WWA), those individuals were excluded from the present study. Since these groups are not represented in this study, these results may not be fully representative of all types of mobility changes following SCI. In addition, while matching allows for a greater control of the factors that contribute to pain severity, it also decreased the study sample size and may not account for all factors that affect pain severity or changes in mobility.
CONCLUSION
Whether a person is walking or wheeling over time does not appear to affect the pain severity; however, differences are present in pain interference. Among those who experience pain, pain interference is more severe among those who use a wheelchair versus those who ambulate at 1-year. Future studies may warrant additional investigation into changes in pain interference over time among individuals who transition in their mode of mobility.
REFERENCES
- Siddall, P. J., McClelland, J. M., Rutkowski, S. B., & Cousins, M. J. (2003). A longitudinal study of the prevalence and characteristics of pain in the first 5 years following spinal cord injury. Pain, 103(3), 249-57. doi:10.1016/S0304-3959(02)00452-9
- Hiremath, S. V., Hogaboom, N. S., Roscher, M. R., Worobey, L. A., Oyster, M. L., & Boninger, M. L. (2017). Longitudinal Prediction of Quality-of-Life Scores and Locomotion in Individuals With Traumatic Spinal Cord Injury. Arch Phys Med Rehabil, 98(12), 2385-92. doi:10.1016/j.apmr.2017.05.020
- Riggins, M. S., Kankipati, P., Oyster, M. L., Cooper, R. A., & Boninger, M. L. (2011). The relationship between quality of life and change in mobility 1 year postinjury in individuals with spinal cord injury. Arch Phys Med Rehabil, 92(7), 1027-33. doi:10.1016/j.apmr.2011.02.010
- Dipiro, N. D., Saunders, L. L., Brotherton, S., Kraft, S., & Krause, J. S. (2014). Pain and fatigue as mediators of the relationship between mobility aid usage and depressive symptomatology in ambulatory individuals with SCI. Spinal cord, 52(4), 316-21. doi:10.1038/sc.2013.164
- Dalyan, M., Cardenas, D. D., & Gerard, B. (1999). Upper extremity pain after spinal cord injury. Spinal cord, 37(3), 191-5. doi:10.1038/sj.sc.3100802
- Pentland, W. E., & Twomey, L. T. (1994). Upper limb function in persons with long term paraplegia and implications for independence: Part I. Paraplegia, 32(4), 211-8. doi:10.1038/sc.1994.40
- Saunders, L. L., Krause, J. S., DiPiro, N. D., Kraft, S., & Brotherton, S. (2013). Ambulation and complications related to assistive devices after spinal cord injury. J Spinal Cord Med, 36(6), 652-9. doi:10.1179/2045772312Y.0000000082
- Turner, J. A., Cardenas, D. D., Warms, C. A., & McClellan, C. B. (2001). Chronic pain associated with spinal cord injuries: a community survey. Arch Phys Med Rehabil, 82(4), 501-9. doi:10.1053/apmr.2001.21855
- Bateni, H., & Maki, B. E. (2005). Assistive devices for balance and mobility: benefits, demands, and adverse consequences. Arch Phys Med Rehabil, 86(1), 134-45. doi:10.1016/j.apmr.2004.04.023
- Krause, J., Carter, R. E., & Brotherton, S. (2009). Association of mode of locomotion and independence in locomotion with long-term outcomes after spinal cord injury. J Spinal Cord Med, 32(3), 237-48. doi:10.1080/10790268.2009.11760778
- Keeler, L., Kirby, R. L., Parker, K., McLean, K. D., & Hayden, J. A. (2019). Effectiveness of the Wheelchair Skills Training Program: a systematic review and meta-analysis. Disability and Rehabilitation: Assistive Technology, 14(4), 391-409. doi:10.1080/17483107.2018.1456566
ACKNOWLEDGEMENTS
The contents of this paper were developed under funding provided by the National Institute on Disability, Independent Living, and Rehabilitation Research (NIDILRR grant number 90SI5014).