Patricia Karg, Amanda Manko, David Brienza, Alexandra Delazio
University of Pittsburgh, Department of Rehabilitation Science and Technology, Pittsburgh, PA
INTRODUCTION
Wheelchair users are susceptible to pressure injury due to a combination of risk factors such as reduced mobility and impaired sensation.[1] Selecting the right seat cushion by matching user needs with cushion performance is paramount to optimizing health and function. Objective information is necessary regarding the performance of cushions that can inform cushion selection to meet individual needs.[2] Over time, cushions experience changes in properties that can impact their ability to properly cushion the buttocks.[3-5] Changes in cushion performance with use must also be considered.
The International Organization for Standardization (ISO) is a non-governmental international organization that develops voluntary consensus standards for seat cushions. RESNA published a national adoption of these standards in 2018, which define performance tests used to characterize cushion properties and minimal methods for simulating cushion aging.[6] This paper presents the effects of simulated aging on the outcomes of a cushion performance test that assesses immersion capabilities. This test was adapted by the Centers for Medicare and Medicaid Services (CMS) as part of its coding verification.
METHODS
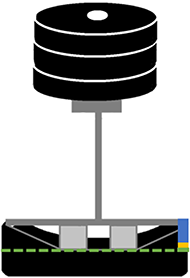
A cohort of 21 cushions of varying constructs were selected to represent general use, skin protection, and positioning cushions available in 2018. Cushions were characterized using 8 performance tests, including Loaded Contour Depth (LCD) and Overload Deflection, which reflects the cushions ability to immerse the buttocks (Figure 1). This test involves loading an indenter that represents a partial pelvis, using cylinders to simulate the ischial tuberosities and greater trochanter bony prominences during seating. The test has three outcomes: (1) Loaded Contour Depth (the depth of immersion of the lowest point of the indenter), (2) Overload Deflection 1 (the additional depth of immersion with a 33% increase in load from the nominal load), and (3) Overload Deflection 2 (the additional depth of immersion beyond the nominal load with a 66% increase in load). Cushions were then aged using the minimum set of simulated aging procedures outlined in RESNA WC-3, Section 6.[6] The following protocol was performed in order: disinfection, laundering, accelerated heated aging, cyclic loading, second round of accelerated heated aging, second disinfection and second laundering. This protocol represents the typical minimum challenges a cushion experiences with use and simulates approximately 18-24 months of actual use. The aging protocol was performed twice on each cushion. The immersion test was performed before and after both aging protocols.
The data was graphed for all cushions for visual comparison. To test differences between means for each metric after each aging cycle, a paired t-test was used for those that met assumptions, otherwise a Wilcoxon signed ranks test was used. In addition, effect size was calculated for each metric. To assess for significant relationships between the change in metrics after aging and cushion subgroups by contour level (none, low, moderate, high), primary material (foam, air, foam+fluid, honeycomb), and general cushion category (general use, skin protection, adjustable skin protection), the data was first recoded into binary variables with foam, skin protection, and cushions without contour used as the reference variables. A linear regression was then used to determine relationships between the categorical data and the change in test metrics. The significance level was set at 0.05.
RESULTS

Test results for the 21-cushion cohort are shown in Figure 2 and Table 1 for the three timepoints: pre-aging, post-aging 1 and post-aging 2. The results of the comparison of means between each timepoint are shown in Table 1. Mean LCD increased after the first aging procedure, then decreased after the second, but changes were not statistically significant. Mean Overload Deflection 1 remained fairly consistent after both rounds of aging. Mean Overload Deflection 2 decreased significantly post aging with a medium effect size. Table 2 indicates significant relationships between the change in the immersion outcome (LCD) after the aging regimens with material constructs of foam only, air only, and foam-fluid hybrids. Significant relationships were also found for the change in the second overload deflection (Overload 2) and cushions with no contour, and with the skin protection subgroup. No significant relationships were found with change in Overload Deflection 1, which is therefore not shown. Figure 3 indicates the changes in LCD immersion after two rounds of aging with the cushions grouped by primary material of construct.
| Variable | Pre-Aging Mean (SD) | Post-Aging 1 Mean (SD) | Post-Aging 2 Mean (SD) | ||
|---|---|---|---|---|---|
| Pre vs. Post 1 p-value | Pre vs. Post 1 Effect Size | Pre vs. Post 2 p-value | Pre vs. Post 2 Effect Size | ||
| Loaded Contour Depth (mm) | 46.3 (15.2) | 48.0 (14.7) | 45.6 (14.5) | ||
| .159 | 0.3 | .639 | -0.1 | ||
| Overload Deflection 1 (mm) | 4.2 (1.7) | 4.0 (1.4) | 4.0 (1.7) | ||
| .545 | 0.1 | .545 | 0.1 | ||
| Overload Deflection 2 (mm) | 8.4 (2.9) | 7.7 (2.1) | 7.8 (2.7) | ||
| .078 | -0.4 | .045 | -0.5 | ||
| Cushion Subgroup | LCD Pre - Post-Aging 1 | LCD Pre - Post-Aging 2 | Overload 2 Pre - Post-Aging 1 | Overload 2 Pre - Post-Aging 2 |
|---|---|---|---|---|
| Foam | .551 | .006 | .181 | .633 |
| Air | .343 | .037 | .362 | .168 |
| Foam + Fluid | .046 | .004 | .354 | .674 |
| Honeycomb | .497 | .073 | .864 | .456 |
| General Use | .621 | .798 | .618 | .203 |
| Skin Protection | .390 | .771 | .571 | .040 |
| Adjustable | .646 | .751 | .537 | .562 |
| Contour: None | .321 | 1.0 | .014 | .026 |
| Contour: Low | .910 | .498 | .058 | .219 |
| Contour: Moderate | .971 | .530 | .398 | .441 |
| Contour: High | .655 | .562 | .106 | .220 |
DISCUSSION

Cushion performance related to pressure injury prevention can be measured, in part, by the ability to immerse the buttocks and distribute weight over a large surface area without concentrations of load. The RESNA Loaded Contour Depth (LCD) and Overload Deflection standardized test method measures immersion using an indenter representing a partial pelvis (including the ischial tuberosities and trochanters). A higher LCD immersion (simulating the immersion of the pelvis) indicates increased capability for pressure distribution. A higher overload deflection indicates additional immersion capability under an overload condition and a higher margin of safety against bottoming out. CMS requires that skin protection cushions have an LCD of at least 4 cm and an overload deflection greater than or equal to 3 mm.
This study aimed to evaluate performance related to these immersion measures following a standardized minimum simulated aging method that represents the minimum challenges all cushions will typically undergo with use. After the first minimum aging procedure, the results showed a small increase in mean immersion (LCD) for the cohort, and a decrease in mean Overload Deflection 2 with a medium effect size. After a second aging procedure was done to assess what further changes may occur, the mean immersion decreased, and there was a significant decrease in mean Overload Deflection 2 with a medium effect size. A decrease in overload deflection after aging indicates a stiffening of the cushion and diminished ability to distribute pressure. This result indicates a user may be at greater risk of pressure injury as their cushion ages.
A previous study that applied loaded contour depth testing to 83 cushions as part of testing for CMS coding found a significant difference in LCD immersion depth occurred post simulated aging.[3] The study found a slight increase in mean immersion after one round of simulated aging, similar to our study. Mean overload deflection (comparable to our Overload Deflection 1) did not change significantly, though eight cushions failed to meet the CMS criterion. The simulated aging method had similar aging procedures to ours (laundering, cyclic loading, heated aging), but were slightly different as they added a partial unloading component and heated aging was for a much shorter period of time. They suggested that the increased immersion from cushion aging resulted in decreased overload protection and increased risk for bottoming out. Another study measured LCD and overload deflection after an average of 35 months real-world use for 55 skin protection cushions, 22% did not meet the CMS overload deflection requirement.[4] Comparing this to our data after two rounds of aging for an equivalent time period, 19% did not meet the requirement.
Figure 3 looks more closely at the change in LCD immersion with aging by cushion and sheds some light on the significant relationships found with general material construct. There was variation in performance based upon material subgroup and within some subgroups. All but one foam cushion had a decrease in immersion while foam + fluid cushions tended to increase in immersion. We explored the significant relationship between the change with aging of Overload Deflection 2 and cushions with no pre-contour (cushions C,D,H,I, L,R,T). The overload deflection decreased for 5 of the 7 cushions.
The study outcomes were limited to the testing of the 21-cushion cohort. Testing of a different or expanded cohort may change the results. Testing of additional commercial cushions is underway to broaden the study. The simulated aging protocol applied was the minimum aging protocol indicated in the RESNA standard. Additional aging challenges such as extreme hot/cold temperatures, soiling, ultraviolet and ozone exposure could impact results.
CONCLUSION
The minimum method for simulated aging as outlined in the RESNA WC-3 standard had a significant effect on cushion performance as measured by the LCD test. Significant relationships were found between the changes in test outcomes and cushion construct and contour level.
REFERENCES
- Sonenblum SE, Sprigle SH. Some people move it, move it… for pressure injury prevention. Journal of spinal cord medicine. 2018 Jan 2;41(1):106-10.
- Hillman SJ, Hollington J, Crossan N, Torres-Sánchez C. Correlation of ISO 16840-2: 2007 impact damping and hysteresis measures for a sample of wheelchair seating cushions. Assistive Technology. 2018 Mar 15;30(2):77-83.
- Linden, M., & Sprigle, S. Changes in Wheelchair Cushions as a Result of Simulated Use Protocols. 2006. 2006 RESNA Annual Conference. Arlington, VA: RESNA Press.
- Rivard DM, Sprigle SH, Linden M. Investigation of the Lifespan for Wheelchair Cushions used on a Daily Basis. 2008. 2008 RESNA Annual Conference. Arlington, VA: RESNA Press.
- Bauer N, Delazio A, Karg P, Brienza D. Visual Characterization of Wheelchair Cushions following Simulated Aging. 2020. 2020 RESNA Conference. Arlington, VA: RESNA Press.
- RESNA. RESNA American National Standard for Wheelchairs - Volume 3: Wheelchair Seating. Rehabilitation Engineering and Assistive Technology Society of North America. 2018. Arlington, VA: RESNA.
ACKNOWLEDGEMENTS
The contents were developed under a grant from the National Institute on Disability, Independent Living, and Rehabilitation Research (NIDILRR grant number 90REGE0001). NIDILRR is a Center within the Administration for Community Living (ACL), Department of Health and Human Services (HHS). The contents do not necessarily represent the policy of NIDILRR, ACL, or HHS, and you should not assume endorsement by the Federal Government.