Building Capability of Allied Health Professionals and Consumers:
A Knowledge Translation Project Using Digital Co-design
L. Callaway,![]() 1,2.3
1,2.3![]() , , E. Bould
, , E. Bould ![]() 2
2![]() & N.Layton
& N.Layton ![]() 1,3
1,3![]()
![]() 1
1 ![]() Rehabilitation, Ageing and Independent Living Research Centre, Monash University,
Rehabilitation, Ageing and Independent Living Research Centre, Monash University, ![]() 2
2![]() Occupational Therapy Department, Monash University,
Occupational Therapy Department, Monash University, ![]() 3
3![]() Australian Rehabilitation & Assistive Technology Association
Australian Rehabilitation & Assistive Technology Association
INTRODUCTION
Mechanisms to put knowledge into practice are an ongoing challenge for allied health practitioners, including in the field of rehabilitation and assistive technology [1-3]. A further dimension is the international paradigm shift toward self-direction within health and disability, and the ongoing pandemic environment, both of which impact knowledge translation activities [4, 5]. The disability academy calls for 'nothing about us, without us' [6,7] and human rights frameworks outline an imperative to ensure meaningful consumer participation in all aspects of human service work (8, 9). Fields such as user-centered design [10], environmental policy [11] and health policy and service design [12] have developed established methods to engage stakeholders.

However, the embedding of consumer voices in the arenas of rehabilitation and assistive technology research are arguably less developed. Engagement can be conceptualized as a 'ladder' of co-production (see Figure 1), and commonly consumers may be informed, consulted or engaged in aspects of policy, service or research processes [13]. The purpose of this project was to use digital co-design and co-production to deliver a suite of accessible online information tools and resources to translate a new allied health capability framework [14] by the Department of Health Victoria, Australia, into practice,
building capability of allied health professionals to work with people with disability who experience complex needs, and of people with disability in selecting and evaluating the quality of allied health services provided to them.
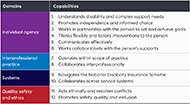
The Framework has been developed for an initial 10 allied health disciplines, and comprises six guiding practice principles (rights-based; person- and family-centred; trauma-informed; recovery-oriented and strengths-based; connected; supportive of Aboriginal self-determination; and responsive to diversity) and 12 capabilities (described as non-clinical skills, knowledge and attributes that show work is being done well), that are operationally defined across foundational, established and leading practice levels (see Figure 2).
As an example of Framework content, Capability 4 (Thinks flexibly and tailors interventions to the person) has a range of sub-categories of operationally defined behaviours and Capability 4.3 articulates three levels of mastery of capacity-building approaches and interventions to enhance a person's capacity and participation, including modifications and assistive technology [14].
METHOD
This project was conducted between March 2020, and December 2020 and was delivered at the height of the pandemic in Australia, with 'lock down' restrictions in place [16]. Thus, captioned videoconferencing and webinars, and other accessible online methodologies, were utilised for all stages of the co-production.
Digital co-design was used, where consumers – termed 'lived experience experts' – were engaged from project commencement for the duration, on a paid basis to work as part of the research team to plan, explore, develop and deliver content and evaluate it [17]. A project team was established with a project lead and manager who had allied health and disability expertise. Three people with lived experience of disability were employed on the project team and another three people with lived experience were contracted for additional digital co-design work. This lived experience expertise was coupled with allied health expertise across occupational therapy, physical therapy, speech pathology, psychology, podiatry and audiology within the project team. The lived experience group worked with the project manager, leading production of video training content in each of the Framework modules for allied health professionals. A suite of digital stories of allied health professionals responding to the lived experience consumer perspectives and reflecting on their own practice across disciplines were also produced, aligned with the various capabilities identified in the Framework.
A series of four co-design workshops were held with the three project team members with lived experience of disability to finalize the resources for people with disabilities and their families, to take for broader consumer and allied health sector review and feedback. Online forums for people with disabilities, their families and allied health professionals (n=85) were then hosted for this feedback and evaluation and to inform the final resource development (see results below). This digital co-creation was coupled with environmental scanning, and existing resource and government policy reviews, the findings of which were made available on a resource tab, one for allied health professionals and one for people with disabilities, their families, friends and carers.
RESULTS
The results from this project have been made available via a free website, called My Allied Health Space (www.myalliedhealthspace.org). My Allied Health Space can be viewed in standard view or Easy Read, and offers an entry point to implementation tools and resources for both allied health professionals and people with disability and their families, friends and carers.
The following suite of free digital outputs were co-constructed (see also Figure 3):
- For allied health professionals: There is a searchable resource centre (see https://www.myalliedhealthspace.org/allied-health-professionals/resources/resource-centre) for allied health professionals with 88 different online information and training resources across various topics relevant to allied health practice with people with disability and complex support needs. A comprehensive online learning management system (see https://www.myalliedhealthspace.org/allied-health-professionals/online-education-modules) for allied health professionals containing modules on the National Disability Insurance Scheme (NDIS), NDIS Quality and Safeguards Commission, the World Health Organization's International Classification of Functioning (ICF), and the four domains of the new Framework, as well as various checklists and tools for allied health provision, professional development planning and supervision (see Table 3 for a list of checklists and tools). It links the 12 capabilities identified in the new Framework to the NDIS Quality and Safeguards Commission Practice Standards, to assist with audit evidence if staff complete a specific module in the system. Each module has introductory content developed by people with lived experience of disability, recorded online in the COVID environment and captioned for accessibility.
- For consumers: There is a website with information resources and tools for people with disability who experience complex support needs, their families and friends, and allied health professionals working with them which can be viewed in standard or Easy Read. Checklist for people with disabilities and families to consider their allied health needs, and questions they may consider asking when choosing allied health services or evaluating those services over time (see https://www.myalliedhealthspace.org/people-with-disability-and-complex-support-needs-friends-family-or-carers/allied-health-supports). Each checklist includes a demonstration by a person with lived experience of disability, again recorded online in the COVID environment and captioned.

A total of 85 people with disabilities and/or allied health professionals (representatives of 9 allied health disciplines) attended online webinar events to provide evaluation feedback on the draft resources developed, with 94% rating resources for people with disability, and 95% rating resources for allied health professionals, as moderately, very or extremely useful (see Table 1). Narrative feedback was incorporated into the final resources produced. The allied health professional online Learning Management System has an embedded evaluation of learning content at the end of each of the 10 education modules, which the learner is required to fill out prior to receiving a certificate of completion of that module. This data will be collected throughout 2021 and reported to the Victorian Government in Australia at key timepoints.
| Project Outcomes | Responses | ||
|---|---|---|---|
| Not at all/slightly useful | Moderately useful | Very/Extremely useful | |
| Overall, how useful the respondent thought the implementation tools and training resources would be for allied health professionals | 5% | 23% | 72% |
| Usefulness of a list of existing online Allied Health training resources (that can be filtered by topic) | 3% | 13% | 84% |
| Usefulness of mapping Framework capabilities to the NDIS Quality & Safeguards Commission quality indicators | 11% | 23% | 67% |
| Usefulness of online learning management system of the new Framework content | 4% | 25% | 71% |
| Usefulness of interactive checklist on the UN Convention on the Rights of Persons with Disabilities | 11% | 23% | 67% |
| Usefulness of an interactive checklist of the ICF Clinician Rating Form | 7% | 28% | 64% |
| Usefulness of online learning management system of NDIS, NDIS Quality and Safeguards Commission and ICF content | 5% | 19% | 76% |
| Usefulness of a self-assessment tool and/or organizational-assessment tool for allied health professional practices | 4% | 12% | 83% |
| Usefulness of videos from lived experience experts on the guiding approaches of the framework | 7% | 27% | 67% |
| Usefulness of videos from lived experience experts on the 12 capabilities within the framework | 7% | 20% | 73% |
| Overall, how useful the respondent thought these resources would be for people with disabilities, families, friends and carers | 6% | 21% | 73% |
DISCUSSION
This project delivered a suite of free online resources for people with disability who experience complex support needs, their families, friends and carers, and allied health professionals working with them. These resources were designed using digital co-production with people with lived experience of disability, drawing on their expertise as paid consultants and via a steering committee. Many of the resources produced can be used in assistive technology practice, or in consideration of services received, and hold international relevance. This methodology was used in the height of the COVID pandemic in Australia in 2020, using mainstream technologies and ensuring the voice of people with disability was central to all implementation tools and training resources produced. Engaging allied health peak bodies and disabled persons organizations early and throughout all stages of the project delivery using teleconferencing or videolink, webinar events and online polling, also ensured that these groups were receptive to the co-design approach used. Regular team meetings with the whole project group via a videolink platform were extremely effective in delivering draft content for review, harnessing feedback, and ensuring the resources produced were co-designed with people with disability and allied health professionals.
References
- Romney W, Bellows DM, Tavernite JP, Salbach N, Deutsch JE. Knowledge Translation Research to Promote Behavior Changes in Rehabilitation: Use of Theoretical Frameworks and Tailored Interventions: A Scoping Review. Archives of Physical Medicine and Rehabilitation. 2021.
- Bowen S. The Relationship between Engaged Scholarship, Knowledge Translation and Participatory Research. 2015 2020/10/05. In: Participatory Qualitative Research Methodologies in Health [Internet]. 55 City Road, London: SAGE Publications Ltd. Available from: https://methods.sagepub.com/book/participatory-qualitative-research-methodologies-in-health.
- Shakespeare T, Kleine I. Educating health professionals about disability: A review of interventions. Health and Social Care Education. 2013;2(2):20-37.
- Pols J. Knowing Patients: Turning Patient Knowledge into Science. Science, Technology, & Human Values. 2013;39(1):73-97.
- World Health Organisation. Coronavirus Disease (COVID-19) pandemic 2020. Accessed via https://www.who.int/emergencies/diseases/novel-coronavirus-2019
- Swain J, French S, Barnes C, Thomas C, editors. Disabling Barriers – Enabling Environments. 2 ed. London: Sage Publications; 2004.
- Cameron C, Moore M, Nutt A, Chambers E. Improving understanding of service-user involvement and identity: collaborative research traversing disability, activism and the academy. Disability & Society. 2019;34(7-8):1312-31.
- Watchorn V, Layton N. Advocacy via human rights legislation - the application to assistive technology and accessible environments. Australian Journal of Human Rights. 2011;17(1):117-38.
- Gould M, Leblois A, Cesa Bianchi F, Montenegro V. Convention on the rights of persons with disabilities, assistive technology and information and communication technology requirements: where do we stand on implementation? Disability and Rehabilitation: Assistive Technology. 2015;10(4):295-300.
- LUMA Institute. Innovating for people: Handbook of human-centered design methods. Pittsburgh (PA)2012.
- Ige J, Pilkington P, Orme J, Williams B, Prestwood E, Black D, et al. The relationship between buildings and health: a systematic review. Journal of Public Health. 2018:fdy138-fdy.
- Hill S, editor. The Knowledgeable Patient: Communication and Participation in Health (A Cochrane Handbook): Wiley-Blackwell; 2011.
- Research for Development Impact Network. Research for All: Making Research Inclusive of People with Disabilities. Australia: CBM-Nossal Partnership for Disability-inclusive Development and Research for Development Impact Network; 2020.
- Departmentn of Health (Victoria) Allied health capability framework: disability and complex support needs 2021 Retrieved from https://www2.health.vic.gov.au/health-workforce/allied-health-workforce/ahcf-disability-complex-support-needs.
- [15] Arnstein S. A ladder of citizen participation. Journal of the American Planning Association. 1969;35(42):216-24.
- World Health Organisation. Western Pacific: Coronavirus Disease (COVID-19) pandemic. 2020. Accessed via https://www.who.int/westernpacific/emergencies/covid-19
- People with Disabilities Western Australia. Connect with Me: Training toolkit for organisations co-designing with people with disabilities. 2020.