Mohsen Makhsous, PhD1,2,3, Susan Taylor, OT1, Deborah Pucci, MPT1, James Bankard3, Lissette Ruberte1,4, Fang Lin, DSc1,2,3
1Sensory Motor Performance Program, Rehabilitation Institute of Chicago
2Depts of Physical Medicine & Rehabilitation, 3Physical Therapy and Human Movement Sciences, and 4Biomedical Engineering, Northwestern University
ABSTRACT
Current strategies for wheelchair prescription include devices that can provide stability, comfort, and functional independence/mobility, while assisting in the prevention of fixed spinal deformities which occur from prolonged static positioning3. These goals, however, are often in conflict with each other. A single commercially available device rarely meets all of these goals simultaneously, resulting in a compromise between a posture that is tolerable and functional for the user and which provides enough stability to accommodate weak or paralyzed muscles5. Given that functional muscles must overcompensate for non-functional or weak muscles during upper extremity tasks, the lack of proper trunk stability can lead to long term consequences, such as spinal deformities and pain. Therefore, pelvic and trunk stabilization devices that can be adjusted when the user deems necessary are essential to provide individuals with spinal cord injury the ability to maintain postural alignment and trunk stability, while still permitting independence with functional tasks and increasing overall comfort 6 .
Keywords: wheelchair seating, stability, adjustability, comfort
BACKGROUND
In the U.S. alone, there are approximately 1.4 million individuals who use wheelchairs full time1. For these individuals, independence from the seated position is a primary concern. Among them, individuals with spinal cord injuries (SCI) at cervical level have altered neuromuscular control, requiring seating devices which provide postural stability while permitting functional independence6. Because current supports often interfere with an individual’s ability to perform activities of daily living (ADL), many wheelchair users opt not to use them, thereby exposing themselves to the negative effects of unsupported seating4. Current technology does not provide a comprehensive back support system which effectively maximizes postural stability2, while permitting functional independence and assisting in the prevention of progressive spinal deformities. Another problem created by a “fixed” seated position is discomfort. Persons with intact neuro-muscular systems assume many positions to avoid sitting in the same posture all the time. However, for persons with SCI, there are virtually no options for user-adjustable wheelchair seating that changes posture, other than tilt and recline.. Unfortunately, tilt and recline seat functions result in limited changes of posture and place the person in positions which remove them from their functional positions. Additionally, these features are generally only available for those who use powered wheelchairs.
METHODOLOGY
 |
|---|
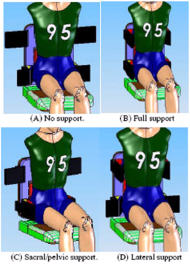
An Adjustable Lumbar-Pelvic-Thoracic Support System ( ALPTS ) was developed for manual and powered wheelchairs (Figure 1) to provide user-controlled postural stability and small changes of posture for function and comfort. It consists of a pneumatic support system that includes: 1) a pair of Postero-lateral pelvic supports, 2) a Lumbo-sacral support, and 3) a pair of Lateral thoracic supports.
Postero-lateral pelvic supports.
Two ABS plastic backing boards with a dimension of 4″×4½″×3/8″ were interfaced with backposts of the wheelchair via two L-shape metal brackets attached at the pelvic level. On each board, an air bladder with a deflated dimension of 4″×4½″×3/8″ was mounted facing the user’s body.
Lateral thoracic supports
Thoracic supports had a similar concept as the pelvic supports. To prevent interference with user transfers from the wheelchair, the thoracic support had a bendable design, which provided not only a strong base for the air bladder, but also enough flexibility for ease of transfers.
Lumbar/sacral support
The lumbo-sacral support had a similar concept as the pelvic supports. Modularity of the lumbo-sacral support was created by attaching strips of Velcro onto the cover of the lumbar/sacral support, which permitted vertical adjustment of the lumbo-sacral support depending on body habitus.
Air Bladders
The air bladders used in this conceptual design were made of natural rubber (Perma-Type Rubber, Plainville, CT). Inflation/deflation of the air bladders could be readily performed by the user via a button switch. Each unit can be individually adjusted in location, tilting angle, and air bladder pressure to provide maximum support and stabilization depending on user’s requirements. In this way, two objectives were achieved: (a) firm support and postural stabilization, and (b) user comfort and body mobility. Furthermore, simple deflation of individual support units provided further mobility of the user if necessary, independent of caregivers. The bendable design of the thoracic support avoided hindering individual wheelchair transfers. Moreover, an air bladder works as a damper of vibration and loads as compared with a solid support during impact.
We evaluated the potential benefits of this wheelchair backrest system with 4 full- time wheelchair users with cervical level SCI (C5/6 to C8/T1) by quantifying the biomechanical effects of the ALPTS in performing upper extremity reaching. We hypothesized that upper extremity function would improve with improved postural stability provided by the ALPTS system.
Reaching tasks:
 |
|---|
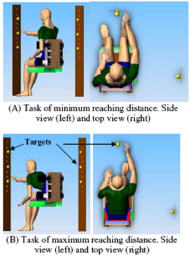
Three targets were placed in front of and lateral to the subject’s right shoulder (all four volunteers were right handed), at 3 levels: shoulder height, 20% higher, and 20%. The subject was then instructed to reach for the targets, one at a time. The tasks were performed when the targets were placed at a distance of the arm length and 30% further.
ALPTS setup :
During each of the above reaching tasks, the ALPTS was setup in 5 different conditions: NONE – none of the air bladder in ALPTS was inflated; PELV – use only the postero-lateral pelvic supports; THOR – use only the lateral thoracic supports; PELV+LUMB – use both the posterio-lateral pelvic and lumbar-sacral support; ALL – use all the supports.
Measurements:
Kinematics and muscle activities from shoulder, upper arm and lower arm were recorded. The kinematics were recorded using OPTOTRAK (OPTOTRAK 3020, Northern Digital, Waterloo, Canada) with active infrared markers. Surface EMG was recorded from four groups of muscles using Delsys EMG system (Delsys Inc, USA): Trunk: lateral portion of the Serratus Anterior, Pectoralis major, and Latissimus Dorsi at T4 and T8 level; Neck-shoulder: both left and right sides of the upper part of the Trapezius and, Sternocleidomastoid; Upper arm: the anterior, medial, and posterior part of Deltoid; Lower arm: the long and lateral heads of the Triceps, Biceps. A common reference electrode was placed at the spinous process of C7. Since cervical level SCI individuals utilize the neck-shoulder muscles to maintain postural stability, muscle activities from this group were recorded from both the sides to evaluate the muscle efforts in maintaining stability.
RESULTS
As expected, the EMG readings and ranges of movement differed, depending on level of injury and other factors, such as the degree of muscular spasms. Main effects were identified as following:
- Less muscle effort was required to maintain postural stability when using the ALPTS system.
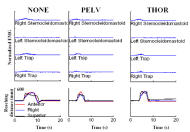
- All subjects demonstrated a consistent pattern of decreased EMG readings on the stabilizing muscles, i.e. trunk and neck, both from the dominant side and the contralateral side. In Figure 3, for accomplishing the task to reach the target at 130% arm length and 120% shoulder height, the muscle activity from the neck-shoulder was less for both sides, when using PELV and THOR. Furthermore, a more even pattern of muscle contraction was seen in neck-shoulder muscles throughout the entire movement, suggesting a decreased need for muscle recruitment.
- A Shorter time period, which varied depending on supports used and activity was required to accomplish the task and a smoother trajectory of movement was seen when using the ALPTS system.
- All subjects required a shorter time period to achieve the same reaching task and a smoother arm movement was seen.
- ALPTS provided comprehensive support, with enough modularity to meet each individual user’s needs.
- It was observed, in some subjects, that inflation of lumbo-sacral support, with postero-lateral pelvic support already inflated, resulted in increased EMG activity of the Sternocleidomastoid and Trapezius. This is probably because that the introduction of the lumbo-sacral support results in rotation of the pelvis from a posteriorly tilted position to a neutral or slightly anteriorly tilted position. However, EMG readings of these muscles decreased with the further introduction of lateral thoracic supports, presumably as they provide trunk stability.
CONCLUSION
Preliminary results suggest that our novel ALPTS system may have a significant impact on providing postural stability and alignment, while permitting mobility to accomplish ADL for wheelchair users with SCI. Feedback from both wheelchairs users and therapists/seating experts was favorable with regards to the ease of using the ALPTS, the ability to provide improved stability, and the ease of adjustment. We believe that more significant benefits will be observed when the wheelchair users use the ALPTS system for a longer time.
REFERENCE:
- Agency for health care policy and research, Pressure ulcers in adults; prediction and prevention, Clinical Guideline no 3. In AHCPR Publ #92-0047. Edited, 1992.
- Alm, M.; Gutierrez, E.; Hultling, C.; and Saraste, H.: Clinical evaluation of seating in persons with complete thoracic spinal cord injury. Spinal Cord, 41(10): 563-71, 2003.
- Hastings, J. D.; Fanucchi, E. R.; and Burns, S. P.: Wheelchair configuration and postural alignment in persons with spinal cord injury. Arch Phys Med Rehab, 84(4): 528-34, 2003.
- Kreutz, D., and Taylor, S.: Seating for the Active Lifestyle. Home health Care Dealer: Sept/Oct. 1994.
- Pedersen, J.; Lange, M.; and Griebel, C.: Seating intervention and postural control. In: Clinician's Guide to Assistive technology, Olsen, d and DeRuyter, F., Eds. Mosby. 2002.
- Sprigle, S.; Wootten, M.; Sawacha, Z.; and Theilman, G.: Relationships among cushion type, backrest height, seated posture, and reach of wheelchair users with spinal cord injury. J Spinal Cord Med, 26(3): 236-43, 2003.
ACKNOWLEDGEMENTS
The project was supported in part by PVA (Paralyzed Veterans of America) Award #2321-01, R24 Rehab Network, NIH Award #R21 HD046844-01A1 and Falk Medical Research Trust.
Author Contact Information:
Fang Lin, DSc
Rehabilitation Institute of Chicago
345 E. Superior St.
Chicago, IL 60611
Office Phone 312-238-4824
EMAIL: f-lin@northwestern.edu