Sharon Eve Sonenblum, MS; Stephen Sprigle, PhD, PT; Leanne West, MS; Jack Wood, MS
Georgia Institute of Technology
ABSTRACT
Erythema, or skin redness, seen after prolonged pressure application is a precursor to pressure ulcers. These occur in people with limited mobility and sensation including the elderly and people with SCI. Erythema is masked by melanin in persons with darkly pigmented skin making it hard to detect.
This study addressed the feasibility of using spectral imaging to detect erythema. Erythema was induced in 32 healthy adults of varying skin color and photographed using 12 narrow-band filters. We mathematically combined the images and applied standard image processing techniques to make the erythema stand out. The results suggest that spectral imaging has potential for detecting erythema. Future work will use automatic optimization to quantitatively calculate the best processing method.
KEYWORDS: pressure ulcer, erythema, spectral imaging, elderly, SCI
BACKGROUND
Pressure ulcers (PUs) are defined as any lesion caused by unrelieved pressure resulting in damage to the underlying tissue (1). PUs are a serious secondary complication for people with impaired mobility and sensation. In 2001, the National Pressure Ulcer Advisory Panel reported prevalence levels in elderly people of 1.5 per 1000 for ages 65-74 and 8.1 per 1000 for ages 75 and older (2). Prevalence of PUs in persons with Spinal Cord Injury (SCI) is reported to be 10-30% at their first annual examination. With annual medical costs in the billions (3) for persons with SCI alone and the resulting decrease in quality of life and potential mortality, the nation’s roadmap to public health, Healthy People 2010, has accurately identified PUs as a considerable public health concern.
Localized erythema, or redness of the skin, is a post-ischemic response that often precedes Stage I PUs. Since the presence of erythema prompts clinical interventions to prevent pressure ulcers, it is vital that erythema is detected. In individuals with darkly pigmented skin, erythema is masked by melanin, hindering early detection of incipient PUs. Research shows greater prevalence of Stage I ulcers in white compared to black patients, but a greater prevalence of Stage III-IV ulcers in black patients (4, 5).
Long-term, this project aims to develop a handheld, clinically-affordable device to identify incipient pressure ulcers. This device will be used by healthcare practitioners to detect erythema in those at risk of developing pressure ulcers. The device will enhance clinicians’ visual assessment of skin.
The current study addressed the feasibility of using spectral imaging in erythema detection. Spectral imaging works like the eye to combine multiple images from overlapping spectral ranges to identify indiscernible targets from complex backgrounds (6). This application is quite similar to detecting erythema (the target) in skin with wide ranging melanin content (the complex background). The technology is inexpensive and non-invasive, as it requires only a camera and narrow-band filters.
METHODOLOGY
Protocol
 |
|---|
Thirty-two subjects were recruited from students, staff and faculty at Georgia Tech. After signing an informed consent form, subjects were asked to shave a small portion of their right leg, just below the knee. Subjects were seated in a lawn chair (Figure 1) so that the height of the imaging system did not need to be readjusted based on subject leg length. The chair supported the subjects’ leg at camera level, roughly 12” from the floor. With the subject seated, erythema was mechanically induced in the area of interest using a custom apparatus. A spherical indenter head was used to apply twenty-four ounces of force to a 1” diameter area for five minutes. The curved head limited edge effects of the indenter on the skin. The indenter was secured with a plastic cuff which could be tightened to increase the pressure applied to the skin. A dial pressure gauge was used to monitor the pressure.
Once the erythema was induced and the cuff removed, the erythema spot was marked with four dots using black eyeliner and a color picture was taken of the erythema area with a Sony Mavica digital camera for reference and comparison to the combined final image.
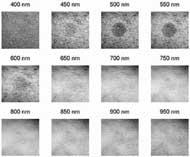
A Grey Dragonfly™ CCD camera, chosen for its broad spectral sensitivity, acquired between 5 and 7 sets of images of each subject. Each set included 12 images taken through non-exclusive filters. Filters ranged from 400–950nm at 50nm increments and a 50-100nm width at half maximum bandwidth. Multiple image sets were taken with varying gain and shutter settings to compensate for the non-uniform spectral response of the camera at these wavelengths. Lastly, a color picture was taken with the Sony Mavica to document how much the erythema had dissipated by the end of data collection.
Analysis
Each image was analyzed using custom Matlab software (Mathworks. Natick, MA). Images were cropped to include a 40 pixel border around the eyeliner markings. The markings were removed from the images by replacing those pixels with pixels from adjacent skin. Each image was equalized, converted to grayscale, and a histogram of the grayscale was generated. For each subject, the best image for each filter was selected as the image with the widest range of values on a grayscale histogram.
For each subject, the 12 images selected – one best image per filter – were loaded into a mathematical weighting program. This program allowed different mathematical combinations of each filtered image to be viewed and analyzed. Algorithms were selected for testing based on knowledge of the chromatic features of the skin and blood.
RESULTS
 |
|---|
Thirty-two subjects were photographed, including 18 Caucasians and 14 African Americans. Two subjects were eliminated from the analysis because the images did not include the entire region of erythema. For the remaining 30 subjects, the 12 best images were analyzed using spectral weighting. Figure 2 shows the 12 best images for a single subject, after cropping and removal of erythema markings. It demonstrates that the erythema stands out in the images filtered in the 450-600nm range.
Two tested algorithms showed the most promise:
Equation 1: (2 ![]() × 550nm - 650 nm)
× 550nm - 650 nm) ![]() × 950nm
× 950nm
Equation 2: (500 nm ![]() × 550 nm) / (600 nm
× 550 nm) / (600 nm ![]() × 650 nm)
× 650 nm)
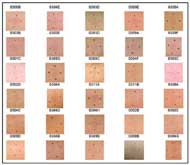
Figure 3 shows the color photographs of the erythema site. Figures 4 a and b illustrate the erythema site after processing with algorithms 1 and 2 respectively, filtering and equalizing the images. The erythema is more obvious in many of the processed pictures. For example, the erythema in dark-skinned Subjects 0309B and 0304C stands out greater when processed by either algorithm. Subject 0304G is improved more by Algorithm 1 while 0308A is helped more by Algorithm 2. Neither algorithm highlights the erythema sufficiently in Subject 0308B.
DISCUSSION
Oxy-hemoglobin (Hb) absorption peaks at 542nm and 574nm; deoxy-Hb peaks at 545nm. Therefore, the erythema is highlighted by the 500nm and 550nm filters. In other words, blue and green filters highlight the red erythema, while the 600nm and 650nm (orange and red) mask the erythema and highlight the melanin and other properties of the skin that clutter the image. The 950nm filter proved useful. This may be because water has a narrow absorption band between 940nm and 970nm (8). Therefore, using the 950nm filter might improve the contrast between areas of erythema with more water content and less reflected light and those without erythema. Additionally, images at this wavelength might identify contrast outside of the visible range of the human eye.
 |
|---|
 |
The images taken with the digital camera were inconsistent with each other because the camera’s lighting and color settings were automated. This presents a limitation to the study because the color digital images could not be accurately analyzed for comparison to the spectral images. Additionally, better lighting conditions might have allowed for fewer image sets (and less time difference between images) and might have provided more data in the 400nm filter.
Overall, this study shows that spectral imaging might be feasible for the non-invasive detection of erythema and prevention of Stage I Pressure Ulcers. Future work will include using a cohort of only dark skinned subjects, capturing clinically presented erythema, and using genetic programming techniques to optimize algorithms and processing for detecting erythema in people of all skin colors.
REFERENCES
- Pressure Ulcers in Adults: Prediction and Prevention. Clinical Practice Guideline No.3. Panel for the prediction and prevention of pressure ulcers in adults., edited by AHCPR, Rockville, MD. US Dept of Health and Human Services, May 1992.
- Pressure Ulcers in America: Prevalence, Incidence, and Implications for the Future. National Pressure Ulcer Advisory Panel, edited by Cuddigan J, Ayello EA and Sussman C, Reston, VA. NPUAP, 2001.
- Krouskop TA. (1983). A synthesis of the factors that contribute to pressure sore formation. Med Hypotheses 11: 255-267.
- Amlung SR, Miller WL, and Bosley LM. (2001). The 1999 National Pressure Ulcer Prevalence Survey: a benchmarking approach. Adv Skin Wound Care 14: 297-301.
- Lyder C, Preston J, Scinto J, Grady J, and Ahern D. (Nov 1998). Medicare quality indicator system: pressure ulcer prediction and prevention module. Final Report. US Health Care Financing Administration.
- Doll TJ, McWhorter SW, Wasilewski AA, and Schmieder DE. (1998). Robust, sensor-independent target detection and recognition based on computational models of human vision. Optical Engineering (special issue on target acquisition modeling) 37: 2006-2021.
- Young K. (May 1994). A study of the accuracy of pulse oximetry among varying skin pigment populations. Long Beach (CA): California State University.
- The Infrared Handbook, Revised edition: The Infrared Information Analysis Center, Environmental Research Institute of Michigan, 1993.
ACKNOWLEDGEMENTS:
Funded by the Georgia Tech Research Institute
AUTHOR CONTACT INFORMATION:
Sharon Eve Sonenblum, MS
CATEA; 490 10 th Street
Atlanta, GA 30318
Phone: (404) 385-0633
Email: Sharon@catea.org