CORRELATING AIR CUSHION PRESSURE TO MAXIMUM INTERFACE PRESSURE ON THE BUTTOCKS
Sean Anderson, Brendon Goede, Daniel Kramer, Maxwell Leupp, Gregory Nemunaitis*, Mohamed Samir Hefzy, and Mehdi Pourazady
Biomechanics and Assistive Technology Lab., College of Engineering, Univ. of Toledo, Toledo, OH *MetroHealth Rehabilitation Institute of Ohio, Cleveland, Ohio
ABSTRACT
Air filled cushions are used to redistribute the interface pressures generated on the boney prominences of the buttocks in individuals who use a wheelchair. However, the method used to determine the proper cushion air pressure to maximize distribution of forces is not accurate, reliable or reproducible. Users are taught to fill their air cushions; sit on it, then let the air out until two fingers fit snugly between the boney prominences of their buttocks and the wheelchair seat. To the best of our knowledge this is the first study that correlates the internal air pressure of the cushion to the interface pressure generated on the buttocks in an attempt to quantify the optimal unloading of boney surfaces on the buttocks. A simple air pressure gauge and an electric pump/bleeder valve combination were used to control the volume of the air in the cushion and to monitor the internal air pressure. Force sensing resistors (FSR) were used to monitor seated interface pressures and alert the user when bottoming out has occurred. This study demonstrated the optimal internal air pressure of ROHO cushion that maximized distribution of seated interface pressures produced over boney prominences while sitting in a wheelchair. In addition, a supplemental foam layer was added below the ROHO cushion to further decrease the interface pressures on the buttocks. The results show that when the internal air pressure of the ROHO is set around 0.6 psi, the interface pressures on the buttocks reduces to about 32 mm Hg which is the maximum pressure that will not cause capillary blood flow impediment (Wilhelmi, 2012).
BACKGROUND
Individuals with spinal cord injury (SCI) are at risk of developing pressure ulcers due to the impairment of sensory feedback over boney prominences on the buttocks. According to the 1998 National Spinal Cord Injury Statistical Center (NSCISC, 1998) Annual Report, 34% of individuals with a SCI developed a pressure ulcer before going home following injury and another 29% developed a pressureulcerbyyear20offollow-upafterinjury.Mostof these ulcers develop in regions that generate high interface pressures on the buttocks due to the boney anatomy of the pelvis. These regions include the sacrum or ischial tuborosity of the pelvis. When seated in a wheelchair repositioning is necessary to unload these pressure sensitive areas and restore blood flow to maintain skin integrity (Garber, et al., 2000). Those that do not remember to weight shift due to the lack of sensation may sit continuously unaware that a pressure ulcer is developing. ROHO (Air filled) cushions are used to help distribute the seated interface pressures over the sitting surface to reduce the focus of pressure, thereby reducing the risk of pressure ulcer formation. A major problem with an air filled cushion is setting the proper inflation air pressure. This is challenging. For example, the instruction manual for one of the ROHO cushions (a ROHO Incorporated Low Profile® Single Compartment Cushion 16" X 16", 9 X 9 Cells, 2" H, Adjustable ROHO) indicates that the air inflation of the cushion must be set so that the lowest bony prominence, usually the ischial tuberosity is one half to one inch from the wheelchair seat. This is done while the user is sitting on a fully inflated cushion and removing air with a goal of allowing the buttocks to submerse within the confines of the cushion until the ischial tuberosity is 1⁄2 to 1 inch from the wheelchair seat. This is very difficult to achieve as the lowest point on the buttocks is generally not visible when seated. Also the usual method of determining the ideal pressure of the air cushion requires the user or caregiver to stick two fingers underneath the buttocks and let the air out until their fingers fit snugly between their buttocks and the wheelchair seat. This is not a very reliable method, especially considering that the user has limited or no sensation on their buttocks, the user may have abnormal sensation or strength in their fingers and another person may have to be available to do this which makes adjustment difficult.
PURPOSE
The purpose of this project is to develop a simple, user independent, and reliable method to adjust the internal air pressure of a ROHO cushion to maximize weight distribution and minimize the focus of pressure on boney surfaces of the buttocks. The closing pressure of arterial capillaries is 32 mmHg or 0.62 psi (1 psi = 51.71 mmHg) which means any pressure higher than this exerted on the capillaries will cause an impediment in the flow. This gives a target for reducing the pressure to as close to 32 mmHg as possible.
METHOD
Several methods have been used to distribute weight and minimize the interface pressure generated on the buttocks of a wheelchair user including using water, gel, foam, memory foam and air cushions. The firmness of the cushion and its comfort level can be adjusted only in water and air cushions. ROHO air cushions are widely used by wheelchair users to reduce interface pressures on boney prominences of the buttock. Accordingly, one of the ROHO cushions was used in this study, namely the Roho Incorporated Low Profile® Single Compartment Cushion 16" X 16", 9 X 9 Cells, 2" H, Adjustable Roho1. In addition the study also tested an additional foam cushion layer underneath the ROHO air cushion to prevent bottoming out. Both systems were coupled with a pressure monitoring system with the air cushion as shown in Figure 1.
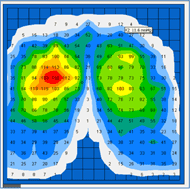
An air pressure gauge was used to monitor the internal air pressure of the ROHO cushion. Through experimentation, the optimal value for internal pressure was determined, requiring the user to only check that the gauge reading was consistent with the optimal pressure found during testing. An analog pressure gauge was used to allow the user to monitor the pressure of the cushion in real time. An air pump was used to inflate the cushion with the push of a button, and a bleeder was used to allow air out of the cushion. A force sensing resistor (FSR) was used to indicate to the user that the pressure inside the cushion is below the acceptable value without having to look at the pressure gauge. The FSR was calibrated to activate an LED light attached to a control box when the pressure on the buttocks was greater than 0.45 psi. Multiple FSRs were laid in series across the cushion in order to ensure that the indicator would go off regardless of the posture of the user. The system included 4 FSRs, 1 high pressure air pump, 1 air bleeder, and 1 control box that was attached to a standard wheelchair as shown in figure 1. A force sensing array (FSA) pressure mapping system (Vista medical, Canada) that shows the amount of pressure (in mm HG) between two contacting surfaces was used to measure the pressure between the subject’s buttocks and the ROHO cushion. The system includes a pressure mapping mat that is placed in between the subject and the air cushion and is interfaced with a computer that has supporting software for the mat. Figure 2 shows a typical pressure map obtained using this system.
RESULTS
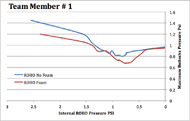
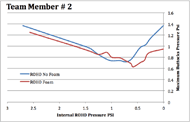
Figures 3 and 4 show how the maximum seated interface pressure on the buttocks changed while changing the internal air pressure of the ROHO cushion. Results are shown with and without the use of an additional foam layer underneath the ROHO cushion. These figures show that the interface pressure on the buttocks decreased from a maximum value when the internal cushion pressure was 0 psi to a minimum value when the internal pressure was around 0.5 to 0.8 psi. These figures show that supplementing the ROHO cushion with a foam layer decreased the maximum seated interface pressure on the buttocks. Similar results were obtained when testing two subjects. The average internal air cushion pressure that corresponded to a minimum seated interface pressure on the buttocks was 0.62 and 0.63psi with and without supplemental foam. The corresponding average maximum seated interface pressure was 0.62 psi and 0.72 psi, respectively, which is equivalent to 31.9 mm Hg and 37.2 mmHg, respectively.
CONCLUSION
To the best of our knowledge this is the first study that correlates the internal air pressure of the ROHO cushion to the seated interface pressure on the buttocks. This study demonstrated the methods to quantify the optimal cushion air pressure that will produce minimal interface pressure while sitting on a ROHO cushion. Finally, this study also demonstrated the effect of adding an underlying foam layer to the ROHO cushion to further decrease the maximum interface pressure on the buttocks. The results show that when the internal air pressure of the ROHO cushion is set around 0.6 psi, the maximum interface pressure on the buttocks is reduced to about 32 mm Hg which is the maximum pressure that will not cause blood flow impediment. Furthermore the cushion could be filled and proper air pressures set with user independence. And finally an additional person was not needed to check the distance from the buttocks to the wheelchair seat while optimal internal air pressure of the cushion was set.
More research needs to be conducted in a clinical setup in order to verify this correlation. Such a task will have a great impact in reducing pressure that may contribute to the formation of pressure ulcers on the buttocks in individuals with spinal cord injuries. Furthermore this system may have further application to individuals that live alone or have significant deficits of motor and sensory function of the upper extremities.
REFERENCES
Wilhelmi, Braden J. (2012). Surgical Treatment of Pressure Ulcers. Medscape reference, WebMD, n.d. Web. 20 Mar 2012.
National Spinal Cord Injury Statistical Center (NSCISC). Model Spinal Cord Injury Care Systems. Annual Report for the Model Spinal Cord Injury Care Systems. Birmingham, AL: NSCISC; 1998.
Garber SL, Biddle AK, Click CN, Cowell JF, Gregorio- Torres TL, Hansen NK, et al. Pressure ulcer prevention and treatment following spinal cord injury: A clinical practice guideline for health-care professionals. Consortium for Spinal Cord Medicine Clinical Practice Guidelines, Paralyzed Veterans of America; 2000.
ACKNOWLEDGEMENT
This work was supported by grant BCS-0931643 from the General & Age Related Disabilities Engineering (GARDE) program from the Biomedical Engineering and Engineering Healthcare cluster of the Chemical, Bioengineering, Environmental, and Transport Systems (CBET) division of the National Science Foundation.
FOOTNOTES
1http://www.medicalsuppliesshop.com/product.cfm/hurl /Low-profile-cushionsingle-valve1675-x-1675-ea.html
Audio Version PDF Version